The number of patients with heart failure (HF) in Japan is estimated to reach 1.3 million by 2030 as the population declines and the proportion of the population aged ≥65 years increases rapidly.1 Approximately 40% of patients with HF are hospitalised within a year and preventing rehospitalisation has become an urgent issue.2,3
In addition to pharmacotherapy, self-care is important for the management of HF.4–6 Self-care in patients with HF is defined as the maintenance of physiological stability by monitoring symptoms, adhering to treatment and selecting behaviours in response to the appearance of symptoms.7 Studies investigating factors associated with rehospitalisation in patients with HF have revealed that medical factors, such as myocardial ischaemia, arrhythmias and infections, as well as factors related to inadequate self-care, such as missed medications, inadequate salt, fluid restriction and overwork, largely contribute to rehospitalisation.8,9 This suggests that it is important to appropriately assess the self-care behaviour of patients with HF and provide relevant support to facilitate improvement.
Self-care behaviour in patients with HF is often assessed using the European Heart Failure Self-care Behaviour Scale (EHFScBS), which relies on self-reporting.10–12 However, self-reported self-care assessments do not always reflect actual self-care performance in this patient group, perhaps because of the high incidence of cognitive decline (25–85%) in older patients with HF.13–18 Nevertheless, there are few studies that have assessed both EHFScBS and actual self-care performance in older patients with HF and ascertained the degree of agreement or the influence of cognitive function.
Guidance could be tailored according to the patient’s abilities to perform self-care, which could contribute to a reduction in hospital readmissions. This could also be useful in identifying patients who should have nursing support at home or who require social care after they are discharged. As most of the previous studies that investigated factors affecting self-care behaviour were based on self-reported self-care assessments, it is unclear which factors are related to actual competence.19–21
This study aimed to compare self-reported self-care assessments and actual self-care practices in older patients with HF stratified by the presence or absence of cognitive decline and to examine the factors influencing the ability to perform self-care.
Methods
Study Population
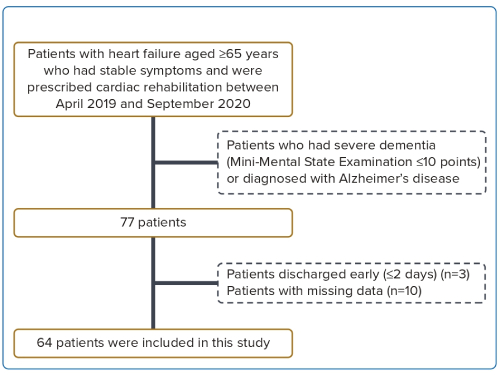
The present study was a single-centre prospective cross-sectional study that included a total of 64 patients with HF aged ≥65 years who were admitted to the Department of Cardiology in Shonan Kamakura General Hospital, Kamakura, Japan and were prescribed rehabilitation and had stable symptoms between April 2019 and September 2020. All participants were informed of the study. The exclusion criteria were as follows: severe dementia (Mini-Mental State Examination – Japanese version [MMSE-J] ≤10 points) and a diagnosis of Alzheimer’s disease.22 The study protocol complied with the tenets outlined in the Declaration of Helsinki and was approved by the Joint Ethical Review Committee of the Tokushukai Group (TGM01184-024). All participants provided verbal and written informed consent regarding participation and publication of data. The participants were informed that they could refuse to participate in the study (Figure 1).
Research Protocol
At the beginning of the study, we explained the pathophysiology and symptoms of HF to patients using a brochure in accordance with the clinical guidelines published earlier and instructed them to avoid behaviours that would aggravate HF (excessive salt and water intake, failure to take medication, overwork and self-interruption of hospital visits).23 Subsequently, the patients were instructed to maintain records related to their daily self-care using the self-management record chart created based on the chart published by the Japanese Heart Failure Society (http://www.asas.or.jp/jhfs/topics/shinhuzentecho.html). The items included in the table were weight, weight gain, blood pressure and pulse, symptoms of HF, rehabilitation, medication status and signs of HF.
Data Collection
The clinical characteristics of the patients, including age, sex, BMI, biochemical data and echocardiographic data, were collected from the electronic medical records at the time of discharge. The clinical details of their presentation and comorbidities were recorded during their hospital stay.
Self-care Assessment
Self-care performance was evaluated as the self-care implementation rate by calculating the percentage of records from the start of the study to discharge using the self-care self-management record chart. The implementation rate was calculated using the percentage of entries for each item in the self-management record chart. Additionally, we assessed whether records were completed without error from medical records; if the medical records were different from those completed, we assumed that they were not properly completed. We also used the EHFScBS, a self-reported HF self-care scale, to evaluate the patients’ self-care behaviours at the time of discharge. EHFScBS is a five-point self-assessment of self-care behaviours related to HF in daily life, consisting of 12 questions scored on a scale of 12 to 60 points. The EHFScBS has been reported to be useful in the assessment of self-care behaviours in patients with HF, with a lower score indicating better self-care performance.10–12
Cognitive Assessment
The Japanese version of the Montreal Cognitive Assessment (MoCA-J) and MMSE-J were used to evaluate cognitive function at discharge.22,24,25 The MoCA-J scores ranged from 0 to 30, with a score <26 suggestive of mild cognitive impairment (MCI). To regulate the effect of education, participants with an educational background of fewer than 12 years were asked to add one score to the total score. The MoCA is well known to be a more sensitive screening instrument for detecting cognitive impairment than the MMSE.25
Measurement of Physical Function Tests
We measured grip strength and the Short Physical Performance Battery (SPPB) score before discharge from hospital. A dynamometer (TKK5101 Grip-D, Takei) was used to measure grip strength. The patient was seated on a bench with their elbow fixed at 90° flexion and performed two maximal isometric voluntary contractions of both hands for 3 seconds each. The width of the dynamometer handle was adjusted to match the patient’s hand size. The greatest strength measured in kg was used in the analyses.
The SPPB comprises a 4-metre usual walking speed, five chair-stand tests and balance tests.26 Each component was scored from 0 to 4 points, and the patient’s lower extremity function was assessed using the total score (range: 0–12 points) with a higher score indicating better functioning of the lower body. In the walking test, patients were allowed to use walking aids, such as canes and walkers.26
Statistical Analysis
Continuous data are expressed as mean ± SD for normally distributed variables and as median with interquartile range (IQR) for non-normally distributed data. Categorical data are expressed as numbers and percentages. The association between the rate of self-management record implementation and EHFScBS was examined using Spearman’s rank correlation coefficient. Additionally, the presence of cognitive decline was stratified using the MoCA-J score of 26 points, which is the cut-off value for MCI.25 The correlation coefficient was calculated. To examine the factors associated with the rate of self-care implementation, we conducted a simple regression analysis investigating the variation factors of the self-care implementation rate and EHFScBS. We also conducted a multiple regression analysis with the significant factors related to the self-care implementation rate and EHFScBS observed in the simple regression analysis as dependent variables. The number of independent variables was calculated by previous studies,27 and six independent variables were used in the multiple regression analysis. Autocorrelation was evaluated by the Durbin-Watson test and the significance level was set at <5%. Statistical analyses were performed using JMP (version 14.1.0, SAS Institute Japan).
Results
Patient Characteristics
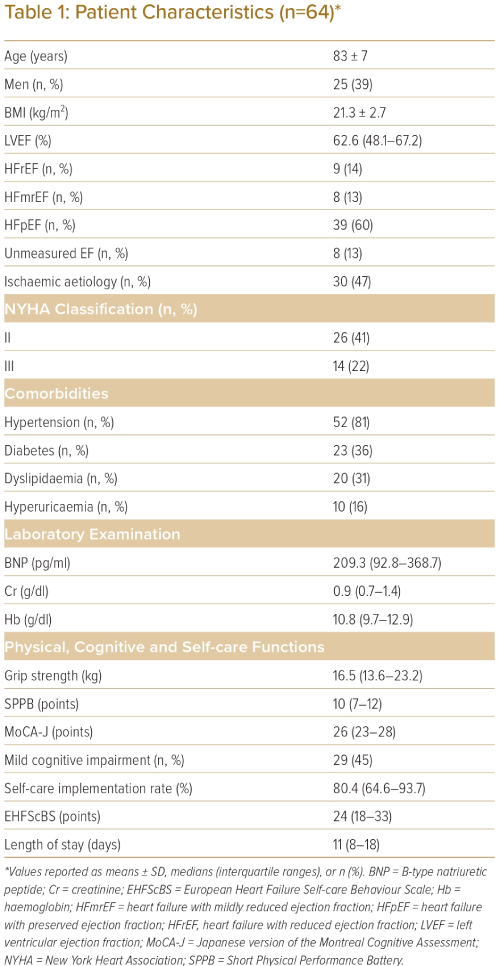
The patient characteristics are summarised in Table 1. After the exclusion of patients according to the stated criteria, 64 patients were included in the study. Of these patients, 25 (39%) were men. The mean age and BMI were 83 ± 7 years and 21.3 ± 2.7 kg/m2, respectively. The prevalence of hypertension, diabetes, dyslipidaemia and hyperuricaemia was 81%, 36%, 31% and 16%, respectively. Ischaemic heart disease was the most common cause of HF (47%) and the median left ventricular ejection fraction (LVEF) was 62.6% (IQR: 48.1–67.2). The prevalence of HF with reduced ejection fraction (HFrEF), mildly reduced ejection fraction (HFmrEF) and preserved ejection fraction (HFpEF) was 9 (14%), 8 (13%) and 39 (60%), respectively. The NYHA classification was II in 41% of the patients. The physical function tests showed that the median grip strength was 16.5 kg (IQR: 13.6–23.2) and the median SPPB score was 10 points (IQR: 7–12). Cognitive function tests revealed a median MoCA-J score of 26 points (IQR: 23–28), which was the cut-off value for MCI. MCI was noted in 29 (45%) of the patients with HF. The median self-care implementation rate was 80.4% (IQR: 64.6–93.7) and the median EHFScBS score was 24 points (IQR: 18–33).
Correlation Between Self-Care Implementation Rate and EHFScBS
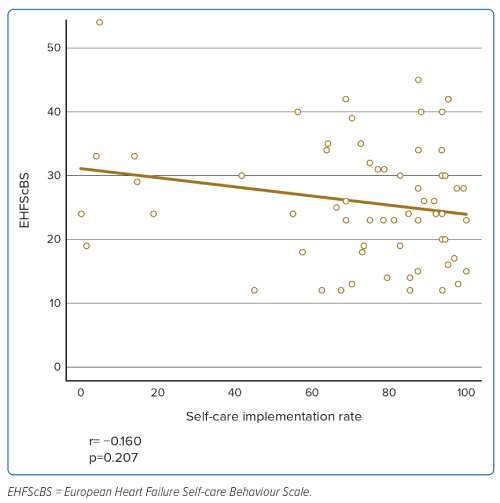
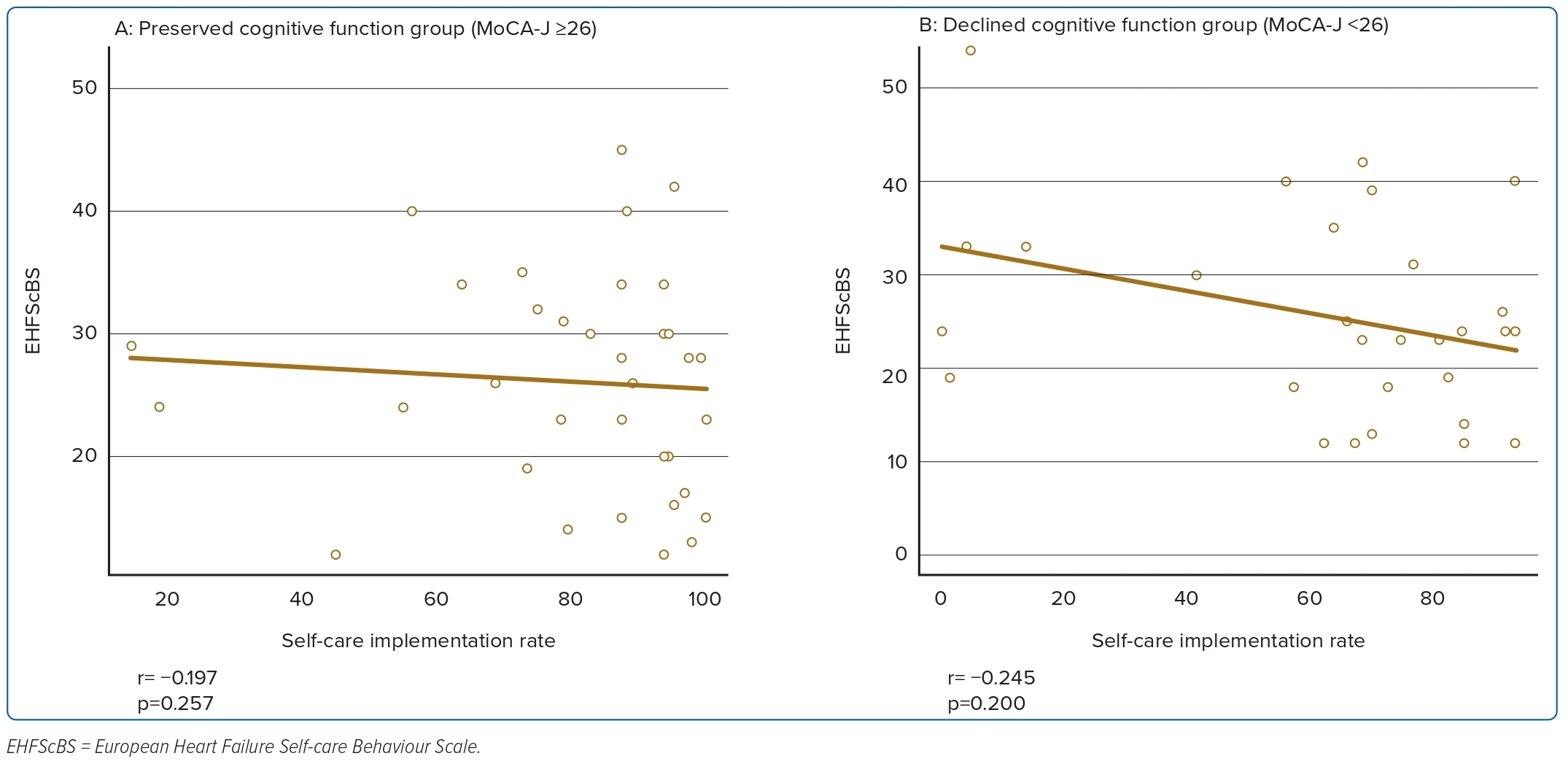
The correlation coefficient between the rate of self-care implementation and EHFScBS was −0.160 (p=0.207); (Figure 2). We also evaluated the relationship between the rate of self-care implementation and EHFScBS, stratified by the level of cognitive function. The correlation coefficients for the groups with preserved and declined cognitive function were −0.197 (p=0.257) and −0.245 (p=0.200), respectively (Figure 3). Supplementary correlations between self-care implementation rate and sub-items of the EHFScBS were also investigated (Supplementary Material Table 1).
Multiple Regression Analysis of Self-Care Implementation Rate and EHFScBS
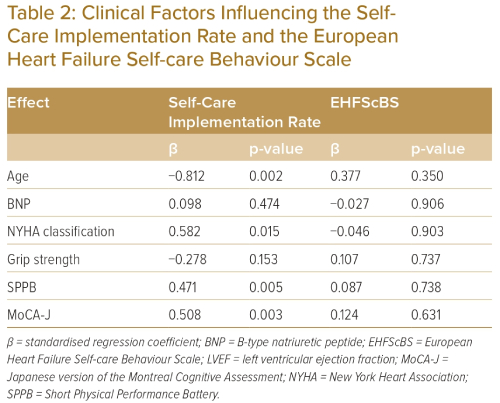
Table 2 shows the results of multiple regression analysis with the rate of self-care implementation as the objective variable. From the results of simple regression analysis, age (p<0.010), grip strength (p<0.010), SPPB score (p<0.010), MoCA-J score (p<0.010), and NYHA classification (p=0.070) were associated with the rate of self-care implementation. Age (p<0.050) and BNP (p=0.070) were also associated with EHFScBS. Multiple regression analysis with these variables was age (p=0.002), NYHA classification (p=0.015), SPPB score (p=0.005), and MoCA-J score (p=0.003) were significantly associated with the rate of actual self-care implementation (Table 2). Older patients with less severe NYHA classification and lower SPPB and MoCA-J scores had lower rates of self-care implementation. There were no factors associated with EHFScBS. The Durbin-Watson ratios were 1.84 for the self-care implementation rate and 2.26 for the EHFScBS. Moreover, these residuals followed a normal distribution.
Discussion
This study examined the correlations between objectively evaluated self-care implementation and EHFScBS, a self-reported HF self-care scale, and factors affecting each self-care measure in older people with HF. The main findings were that there was no significant correlation between actual self-care implementation and EHFScBS and the same results were obtained when stratified by the presence or absence of cognitive decline. Physical and cognitive function were significantly associated with the rate of actual self-care implementation, but there were no factors related to EHFScBS.
This study provides an insight into the discrepancy between self-reported self-care and actual self-care behaviour in older patients with HF, irrespective of cognitive decline.
Previous studies examining the usefulness of EHFScBS have reported that it correlates with other questionnaires with similar constructs.11,12 A previous study found there was almost no association between the reported self-care behaviour (EHFScBS) and observed ability for self-care.28
Factors associated with EHFScBS were also examined. This study showed that there were no factors associated with EHFScBS, including age and cognitive function. Previous studies on factors related to self-care in patients with HF have reported that age, sex, educational background, NYHA classification and physical and cognitive functions were influential factors.18,20,29,30 Particularly, cognitive decline is believed to have an important impact on the performance of self-care, but the lack of significant association between cognitive function and self-reported self-care behaviour scales in this study may be related to the fact that EHFScBS does not reflect actual self-care behaviour. Considering that most patients with HF are older, there is a limit to evaluating self-care using the conventional method of self-reporting and it is important to use an index that evaluates self-care based on actual implementation.
In this study, age, NYHA classification, SPPB and MoCA-J score were significantly associated with the rate of actual self-care implementation; older patients with less severe NYHA classifications and lower SPPB and MoCA-J scores had lower rates of self-care implementation. The effects of ageing may include decreased function in the sensory organs, which may reduce sensitivity in recognising symptoms and may delay the instigation of coping behaviours that support treatment.31
Regarding cognitive function, it has been reported that HF exposure itself is associated with a decline in attention, executive function, working memory, processing speed and visuospatial ability.32 A decline in working memory and processing speed may interfere with the integration and interpretation of knowledge and the performance of self-care.
An earlier study that examined whether education on self-care and HF disease management in hospitalised HF patients with MCI could prevent rehospitalisation 30 days after discharge revealed that although patients with MCI could improve their knowledge, it did not affect their actual self-care behaviour or reduce the rehospitalisation rate.33 Therefore, it is expected that even mild cognitive decline could cause difficulties with self-care.
Study Limitations
This study has some limitations. First, given that this was a single-centre study including hospitalised patients with HF, it was difficult to examine the effects of regional and racial differences. However, an epidemiological study in Japanese subjects showed that patients with HF were older and had lower BMI, consistent with observations in other Asian populations.34,35 Therefore, our results could be extrapolated to Asian patients with HF. Second, the EHFScBS – a self-reported self-care scale used in this study – includes several assessment items, which are challenging to perform during hospitalisation, such as salt reduction and infection prevention. Therefore, we could not accurately assess whether patients could perform all the self-care activities that are necessary to manage HF while they were still in hospital. However, recently published guidelines from the European Society of Cardiology (ESC) for the diagnosis and treatment of HF, in addition to their class I self-management strategies recommendation, have recommended that medical staff should provide training to patients regarding home-based and clinic-based programmes during hospitalisation to reduce the risk of HF rehospitalisation and mortality.36
This study investigated whether patients are aware of living at home and truly capable of performing self-care during hospitalisation. These results are an important survey because they allow healthcare providers to assess whether self-care is feasible early on and determine the patient and their family’s need for guidance and services based on its implementation. Finally, the sample size for this study was small and it was not possible to examine all variables related to self-care, such as educational level and social status. It also did not have a control group and it was not clear whether the instruction of self-management during hospitalisation affected HF rehospitalisation. Therefore, further research is needed to determine whether patients are adequately capable of performing self-care.
Conclusion
In older patients with HF, the self-reported assessment of self-care did not reflect actual self-care performance and results were similar regardless of the presence or absence of cognitive decline. Additionally, age, HF symptoms and physical and cognitive functions affect the actual implementation of self-care; therefore, it is necessary to individualise the content and amount of self-care instructions according to each patient’s background. There is also a need to develop reliable self-care behaviour scales to measure the effectiveness of education for patients with HF. 
Click here to view Supplementary Material
Clinical Perspective
- Mild cognitive impairment was noted in 45% of older patients with heart failure.
- No association was noted between the actual and reported self-care rates.
- Age, heart failure symptoms and physical and cognitive functions were related to actual self-care.
- No factors were related to reported self-care.