Double orifice mitral valve (DOMV), which was initially described by Greenfield in 1876, is a rare congenital malformation that occurs in about 0.05% of the general population.1,2 It is characterised by a mitral valve with a single fibrous annulus, resulting in two orifices.
Its embryonic development, as with most cardiac lesions, is incompletely understood and remains controversial.3 Theories include abnormal embryonic fusion of the mitral leaflets, abnormal fusion of the endocardial cushions or incomplete fusion of the two atrioventricular endocardial cushions.
The most accepted classification for DOMV was described by Trowitzsch et al. in 1985, which defines three types: complete bridge (15%), incomplete bridge and hole type (85%).4
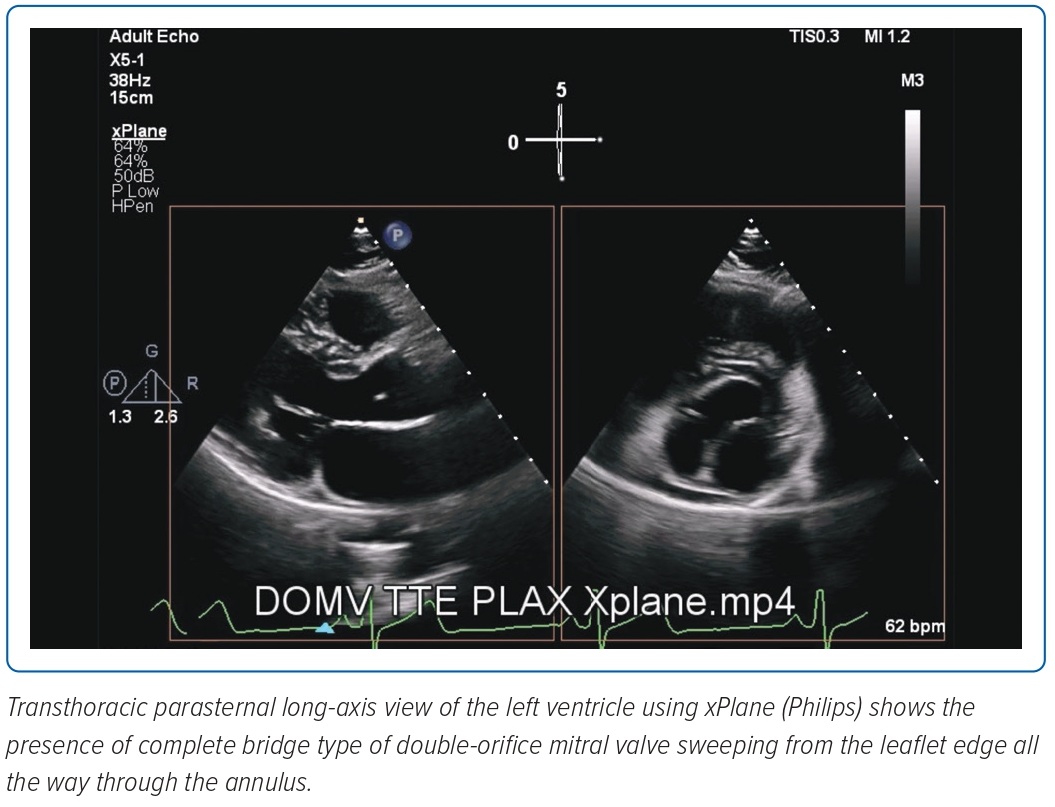
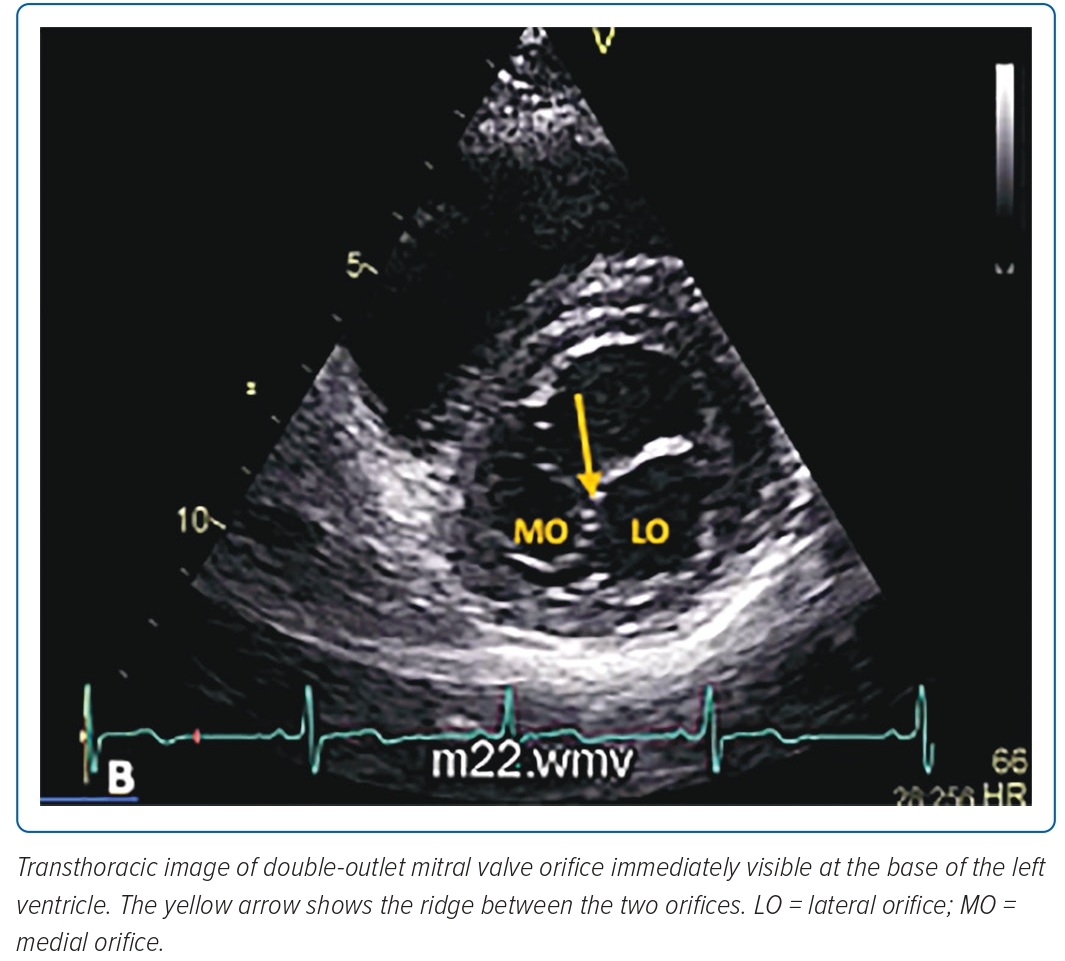
In complete bridge type, both orifices are visible from the leaflet edge all the way through the annulus. Both openings are circular and can be of unequal size. The papillary muscles are usually normal, with chordae surrounding each orifice and inserting into one of the papillary muscles. Incomplete bridge type has a connection only at the leaflet edge and appears normal in the more basal views. The hole type is characterised by a small accessory orifice situated at either the anterolateral or posteromedial commissures. It is visible only at the mid-leaflet level and disappears on scanning toward the apex or base.1
Among the types of DOMV, the hole type is the most common, accounting for 85% of cases. Also known as the eccentric type, it is commonly associated with cardiac anomalies involving the valve apparatus as well as the presence of an atrioventricular septal defect.5
DOMV may occur as an isolated anomaly but, in most cases, it is associated with other congenital malformations.6 Isolated DOMV is extremely rare and its exact incidence, prevalence and prognostic relevance have not been established.7,8
To the authors’ knowledge, this is the first Philippine documentation of an isolated DOMV. In addition, it is the first case to be reported in an adult Filipino patient, as majority of the registries are comprised of paediatric patients with DOMV associated with concomitant congenital anomalies.8
We present a rare case of an isolated congenital DOMV in a 26-year-old Filipino man, diagnosed incidentally by 2D echocardiography, with the diagnosis supported by 3D transoesophageal echocardiography (TOE).
Case Study
A 26-year-old man, a seafarer, was referred to our institution for a pre-employment evaluation. Apart from one episode of palpitations which was allegedly triggered by drinking three cups of coffee, he was apparently well. There had been no recurrence of palpitations thereafter and he denied any associated symptoms. The medical history and physical examination were unremarkable.
A series of examinations were requested. Chest X-ray and 12-lead ECG were normal. His 24-hour Holter report documented 22 premature atrial contractions occurring singly and some in couplets. Treadmill exercise test was normal at 12.8 METS and showed average functional capacity for age and sex. Incidentally, his 2D TTE showed a finding of a DOMV.
A complete 2D TTE with colour Doppler examination using the Epiq 7 (Epiq) showed a DOMV. In the parasternal long-axis view using X-plane and sweeping from the mitral annulus to the leaflet, two asymmetric orifices were visualised (Figure 1).
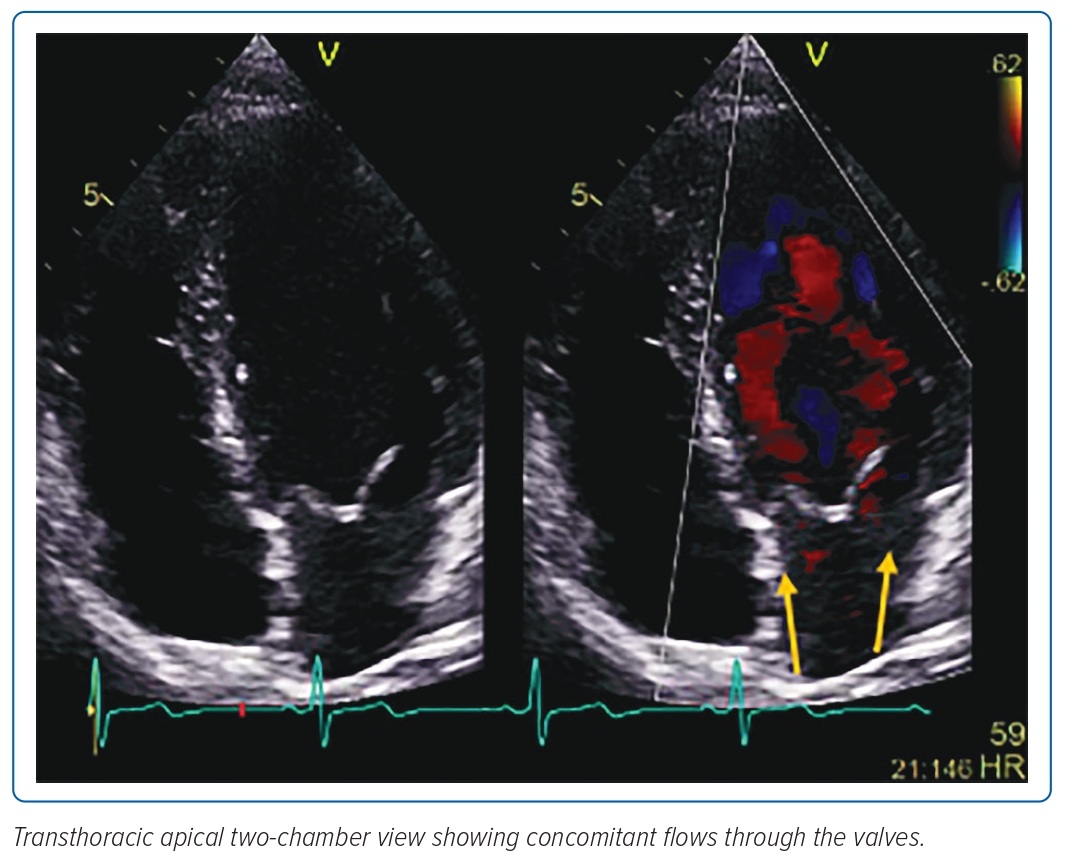
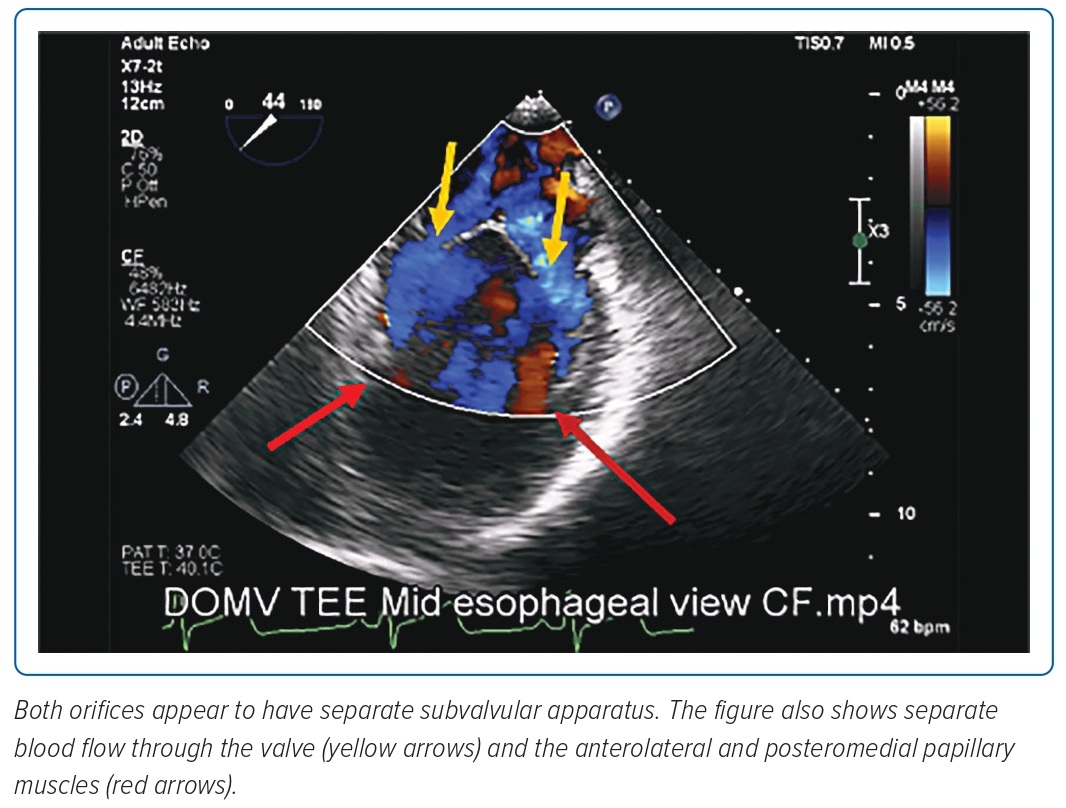
A view of the mitral valve on the apical two-chamber view showed concomitant flows through the valves (Figure 3). The recorded mean gradients across the medial and lateral orifices were 2.6 mmHg and 3.2 mmHg, respectively.
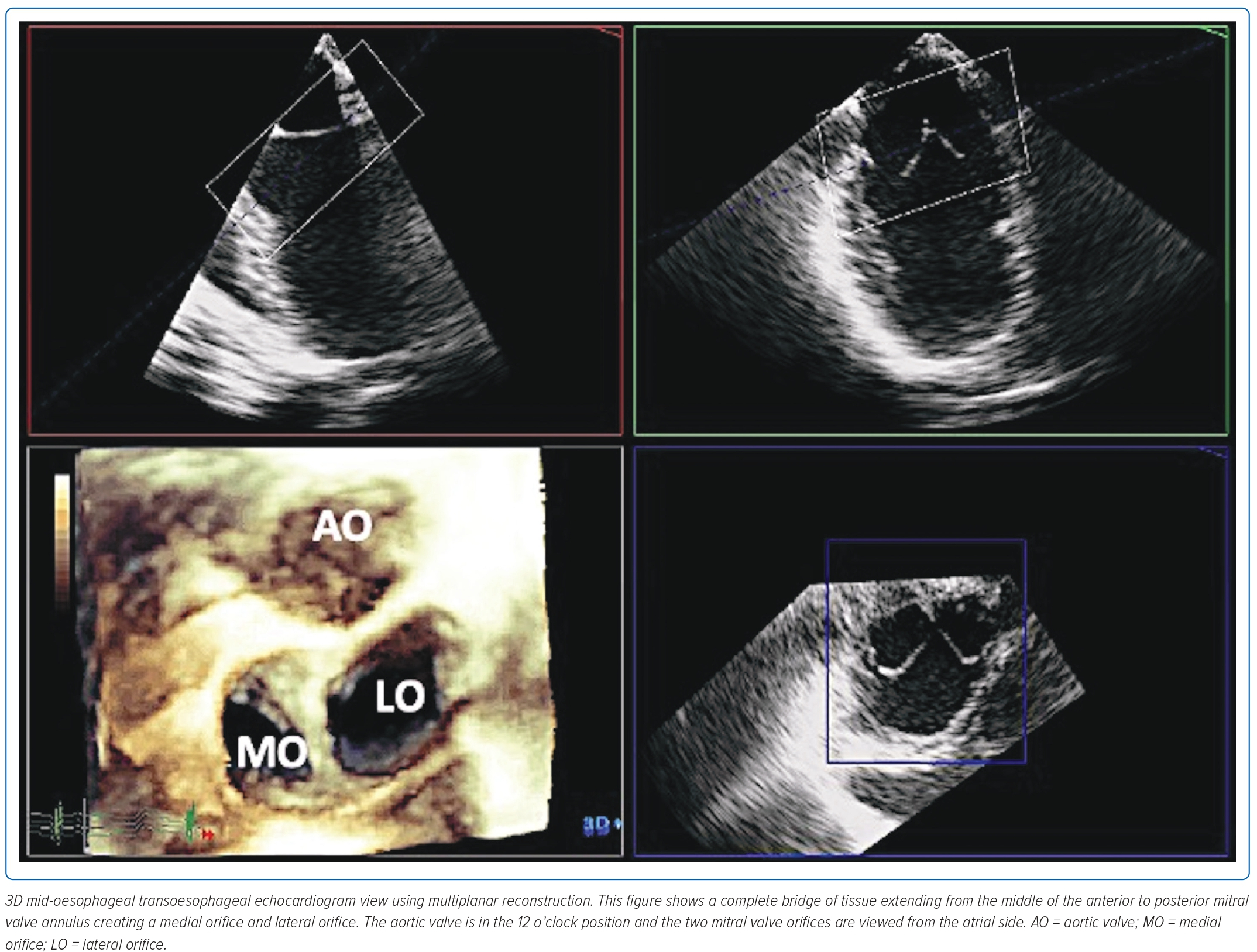
Additional imaging using 2D/3D TOE was done for comprehensive examination of the mitral valve apparatus to rule out any associated cardiac anomalies.
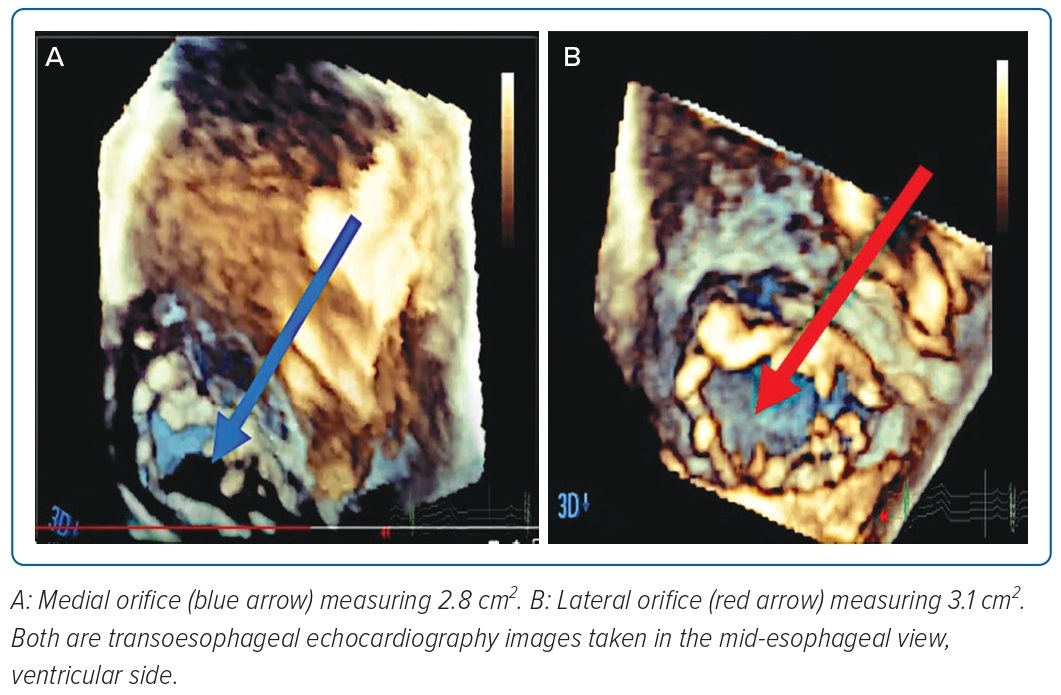
On mid-oesophageal view, a complete ridge of tissue was noted extending from the middle of the anterior to posterior mitral valve annulus creating a medial and lateral orifice (Figure 4). 3D multiplanar reconstruction showed that both orifices had two leaflets, each with a good opening and closing motion (Figure 4). A mild regurgitant jet was noted in the lateral orifice. Using 3D multiplanar reconstruction, the mitral valve area of the lateral orifice was measured at 3.1 cm2, while the medial orifice was measured 2.8 cm2 (Figure 5).
On further examination, both the interatrial and interventricular septa are intact. There was no cardiac chamber enlargement and the remaining cardiac valves were structurally normal with physiologic regurgitation in the tricuspid valve.
Images taken from the mid-oesophageal view showed that both orifices appeared to have separate subvalvular apparatus (Figure 4). Two papillary muscles were identified (anterolateral and posteromedial), both giving off chordae attached to the leaflets. (Figure 6).
Discussion
DOMV is a rare cardiac congenital anomaly characterised by a mitral valve with a single fibrous annulus and two orifices. A literature search using HERDIN Plus showed no local published reports of isolated DOMV in adults.8
The purpose of reporting this case is to provide information to help identify DOMV by using 2D and 3D imaging since there are no published cases in our local setting to the best of our knowledge.
As reported by Baño-Rodrigo et al., in a large autopsy series of patients with congenital heart disease, 1% had a DOMV, and in the majority of cases this was associated with other cardiac anomalies (atrioventricular septal defect, coarctation of the aorta, patent ductus arteriosus or interrupted aortic arch) or mitral regurgitation.9
Because of the associated anomalies, DOMV is usually detected in early childhood, but is hardly ever diagnosed in adults, so the incidence and prognostic relevance of an isolated DOMV detected in adulthood is unknown.7
Cases of an isolated DOMV with no functional abnormalities are likely to be missed because there will be no clinical symptoms. Recognition of DOMV and awareness of the anatomic variations are important to achieve good therapeutic results. Treatment is necessary only if significant mitral stenosis or mitral regurgitation is present.5
DOMV is usually detected by 2D echocardiographic examination in short-axis parasternal views. However, information obtained by 2D echocardiography may not be sufficient to enable identification of the different types of DOMV.6 Performing 3D echocardiography is useful in identifying the morphology type and providing further anatomical and functional information, such as orifice size, number of leaflets and spatial relationship, and identifying associated congenital heart anomalies that had not been seen in transthoracic 2D echocardiography.10,11
In cases in which transthoracic 2D images are suboptimal and TOE echocardiogram is not an option (i.e. it is contraindicated or not the patient’s preference), cardiac MRI can be an alternative choice.12,13
Our patient had the complete bridge type of DOMV, presenting with two unequal circular orifices, both with their own set of leaflets, commissures, chordae and papillary muscles as documented by an echocardiogram.
Another feature associated with this congenital anomaly, aside from possible concomitant structural cardiac abnormalities, is arrhythmia.14 Both AF and atrial flutter have been documented in some cases of DOMV. These have been attributed to chronic left atrial enlargement secondary to mitral stenosis or mitral regurgitation physiology.5 In our case, supraventricular ectopic beats were documented.
Management would depend on the severity of the valvular stenosis and/or regurgitation, associated congenital defects and clinical presentation. Asymptomatic DOMV usually requires no active intervention; in cases of severe mitral regurgitation, stenosis or associated cardiac anomalies, surgical repair is needed.15
In our case, as symptoms and concomitant abnormalities were absent, regular long-term follow-up was advised for the early detection of complications and no active medical or surgical intervention was warranted.15 
Clinical Perspective
- Double orifice mitral valve (DOMV) is a rare cardiac congenital anomaly characterised by a mitral valve with a single fibrous annulus and two orifices.
- Recognition of double-orifice mitral valve and awareness of the anatomic variations are important to achieve good therapeutic results. Treatment is necessary only if significant mitral stenosis or mitral regurgitation is present.
- Another feature of this congenital anomaly, aside from possible concomitant structural cardiac abnormalities, is arrhythmia. Both AF and atrial flutter have been documented in some cases of DOMV. This has been attributed to chronic left atrial enlargement secondary to mitral stenosis or mitral regurgitation physiology. In the case described here, supraventricular ectopic beats were documented.
- Management depends on the severity of the valvular stenosis and/or regurgitation, associated congenital defects and clinical presentation. Asymptomatic DOMV usually requires no active intervention; in cases of severe mitral regurgitation, stenosis or associated cardiac anomalies, surgical repair is needed. In the case discussed here, because there were no symptoms and concomitant abnormalities, regular long-term follow-up was advised for the early detection of complications.











Comments