Acute MI (AMI) is one of the leading causes of morbidity and mortality in the Philippines and worldwide. Across the AMI spectrum, ST-elevation MI (STEMI) carries the highest risk.
Mortality due to STEMI is influenced by various factors, including advanced age, Killip class, treatment strategy, history of AMI, diabetes, renal failure, number of diseased coronary arteries, left ventricular ejection fraction, and time delay to treatment.1 The primary goal in the treatment of STEMI is prompt revascularisation with the shortest possible ischaemic time.
Delays in STEMI treatment can be attributed to three types of factors: patient-related, system-related and procedural. Patient delays often occur due to insufficient awareness, misinterpretation of symptoms, logistical traffic and financial constraints, particularly in developing countries.2
Developed countries typically have an emergency medical system in place, assisting with prehospital diagnosis, treatment, and transportation to a percutaneous coronary intervention (PCI)-capable hospital. However, even in these countries, delays can still occur due to patient-related factors, such as the absence of chest pain, dyspnoea as a symptom and long distances from the scene to the hospital.3
The Philippines government and health sectors advocated for increased AMI awareness to reduce patient delays. However, limitations in recall bias regarding the exact time of chest pain onset make it challenging to establish the true time of AMI.4 Procedural delays, on the other hand, can arise from operator-related and patient anatomy-specific problems, making them difficult to predict or control. Cases involving challenging vascular access and lesion crossing are examples of delays associated with in-hospital mortality.5 In contrast, system delays, which refer to the time from first contact with the healthcare system to initiation of reperfusion therapy, can be readily analysed and improved. These delays have been shown to impact mortality.6 Efforts to reduce system delays rely on regular analysis and implementation of targeted solutions for each specific component.
The European Society of Cardiology guidelines recommend the new STEMI diagnosis to wiring time of 60 minutes over the traditional door-to-balloon (DTB) time of 90 minutes. However, both are measurable parameters for predicting early and long-term outcomes.1,7,8 The limitation of the DTB time goal lies in differences in interpretation and changes in context depending on the subject. The DTB is also prone to false-positive activations due to inadequate evaluation in the emergency room (ER), leading to unnecessary PCI.9 This is the reason why the STEMI diagnosis-to-wire cross time has gained wider acceptance.
A STEMI response and AMI programme was initiated in 2012 at The Medical City, a private tertiary care hospital, and has been accredited by the Joint Commission International. In The Medical City’s AMI programme, the time goals are segmented into different time frames for the purpose of audit, improvement and quality control. The COVID-19 pandemic has resulted in longer STEMI delays, as reported in other studies, making it crucial to implement initiatives for system improvement.10,11 While all staff and departments involved in the STEMI response and AMI programme are aware of the 60- and 90-minute goals, it is also important to establish optimal target points for each time frame to enhance the likelihood of achieving the established goals.
Objectives
The objectives of this study were to determine hospital delays in the STEMI response programme and to set target points in every time frame that could be used to increase the chances of meeting the DTB time and STEMI diagnosis-to-wire cross goals.
Methods
This retrospective cohort study included all adult patients aged ≥19 years who presented to The Medical City’s ER and were subsequently enrolled in the AMI registry due to STEMI. The patients were treated with emergency PCI by five interventional cardiologists (IC) based on a round-the-clock schedule, with morning and evening decking, 24 hours a day, 7 days a week, between January 2019 and June 2021.
Participants included those who arrived at the ER via private transport or by independent ambulance without a prehospital 12-lead ECG. Patients with pre-diagnosed STEMI who were transferred from other hospitals were excluded from the study. The data collected from the AMI STEMI registry included age, sex, time of arrival (whether office or non-office hours) and time frames in minutes.
The different time frames began with the door to ECG time, measuring the duration from the patient’s arrival, as logged in the information technology suite, to the printing of the first 12-lead ECG. When a STEMI diagnosis was suspected, the ER resident paged the cardiology fellow on duty (CFOD), representing the ECG to paging time. The paging to CFOD arrival time indicated the interval it took for the CFOD to arrive in the ER from another location after being paged. The CFOD arrival to STEMI diagnosis time captured the interval it took for the CFOD to make a diagnosis based on symptoms consistent with MI and typical or atypical ST-elevation ECG criteria. Subsequently, the study recorded the interval from STEMI diagnosis to the signing of a consent form by the patient or their relatives for emergency PCI, patient consent to the patient’s arrival in the cardiac cath lab and, finally, the time from arrival in the cath lab to the initiation of vascular access (‘puncture’).
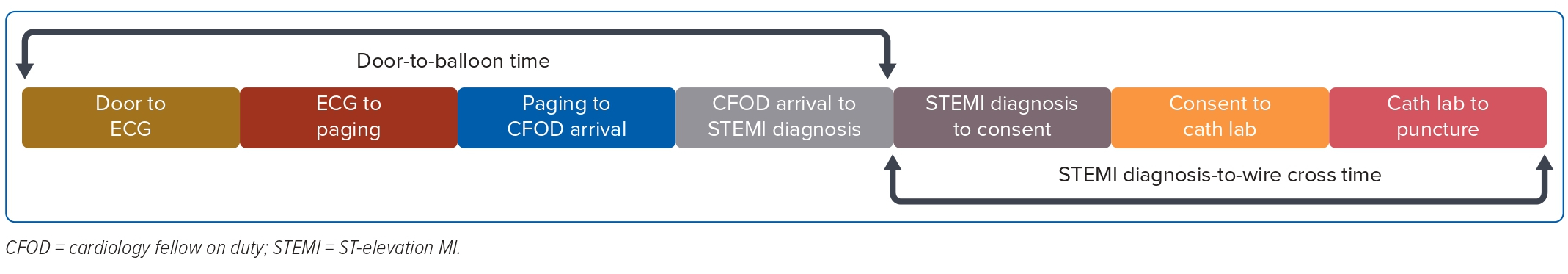
The DTB (i.e. first balloon inflation of the culprit artery) and STEMI diagnosis-to-wire cross (i.e. from STEMI diagnosis to wire crossing of the infarct-related artery) times were divided into Met and Unmet groups using targets of ≤90 and ≤60 minutes, respectively, in the Met group and >90 and >60 minutes, respectively, in the Unmet group. The different time frames were grouped into DTB and STEMI diagnosis to wire cross based on their involvement in the STEMI treatment goals (Figure 1). Optimal target points were obtained for each time frame.
Data Organisation, Editing, Processing and Analysis
Data obtained were checked for completeness and categorised into four groups using Microsoft Excel (version 16.30) as follows:
- Met DTB goal of ≤90 minutes.
- Unmet DTB goal (>90 minutes).
- Met STEMI diagnosis-to-wire cross goal of ≤60 minutes.
- Unmet STEMI diagnosis-to-wire cross (>60 minutes).
Data were rechecked twice to ensure correctness and validity.
Statistical Analysis
Descriptive statistics were utilised to summarise the demographic and clinical characteristics of the patients. Categorical variables were presented as frequencies and proportions, while non-normally distributed continuous variables were presented as the median and interquartile range (IQR), and normally distributed continuous variables were presented as the mean ± SD. Independent sample t-tests, Mann–Whitney U-test, and Fisher’s exact/χ2 test were used to determine the significance of differences in mean, rank, and frequency values between groups with met and unmet DTB and STEMI diagnosis-to-wire cross time goals. For time frames that did not exhibit significant differences, the median of the Met group was considered as the optimal target point. In the case of time frames that did differ significantly, optimal target points were selected based on achieving the highest possible percentage of Met and Unmet cases, using a goal of either DTB time of 90 minutes or STEMI diagnosis-to-wire cross time of 60 minutes. Binary logistic regression was conducted to compute ORs and corresponding 95% CIs to determine whether the target point of the time frames predicted an unmet status during DTB and STEMI diagnosis to wire cross.
All statistical tests were two-tailed. The Shapiro–Wilk test was used to test the normality of distribution of continuous variables. Missing values were neither replaced nor estimated. Null hypotheses were rejected at an alpha level of 0.05. Stata 13.1 was used for data analysis.
Results
From January 2019 to June 2021, a total of 113 patients with STEMI who underwent emergency PCI were included in The Medical City’s AMI STEMI registry. Figure 1 illustrates the time frames used for DTB and STEMI diagnosis to wire cross. The majority of patients (73.45%) did not meet the DTB goal of 90 minutes, and there was a significant difference in DTB time between the Unmet and Met groups (median 141 minutes [IQR 111–216 minutes] versus 70 minutes [IQR 64–90 minutes], respectively; p≤0.001).
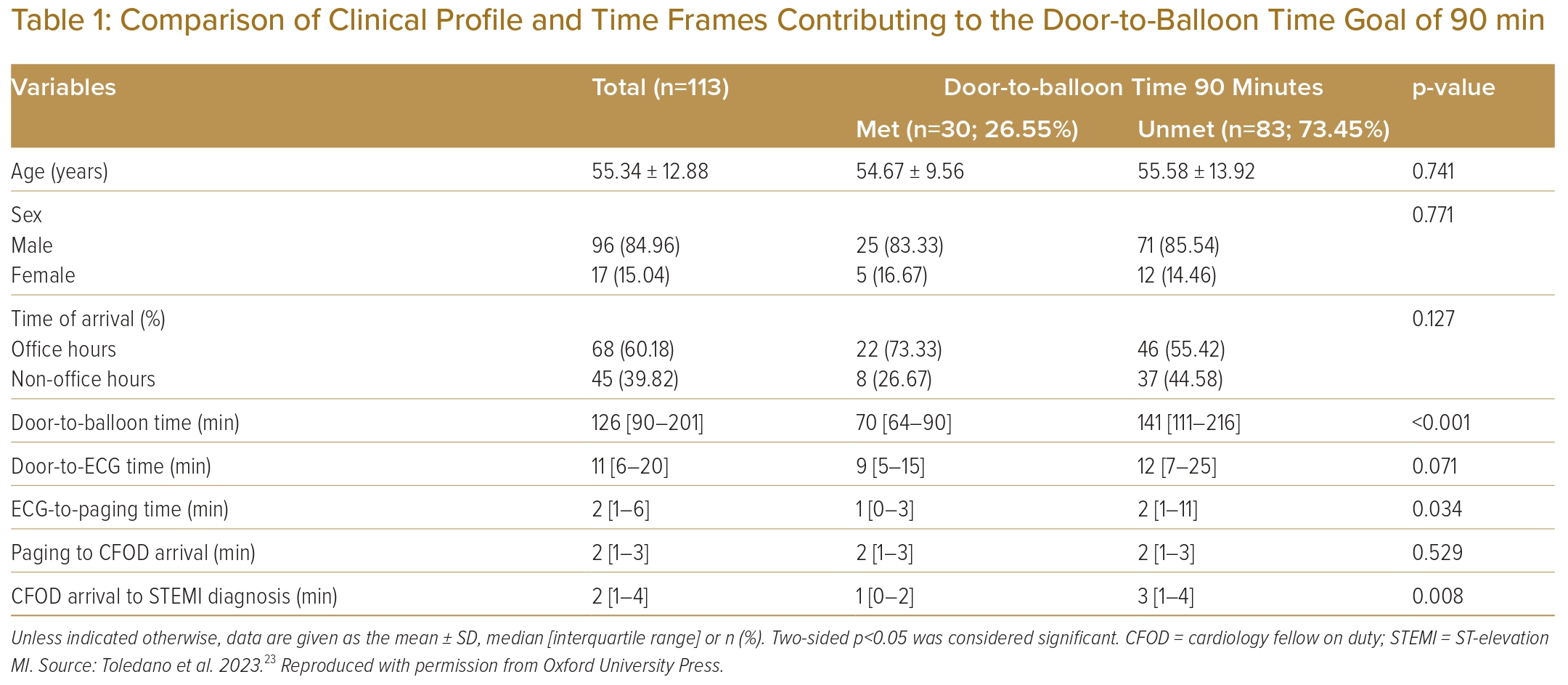
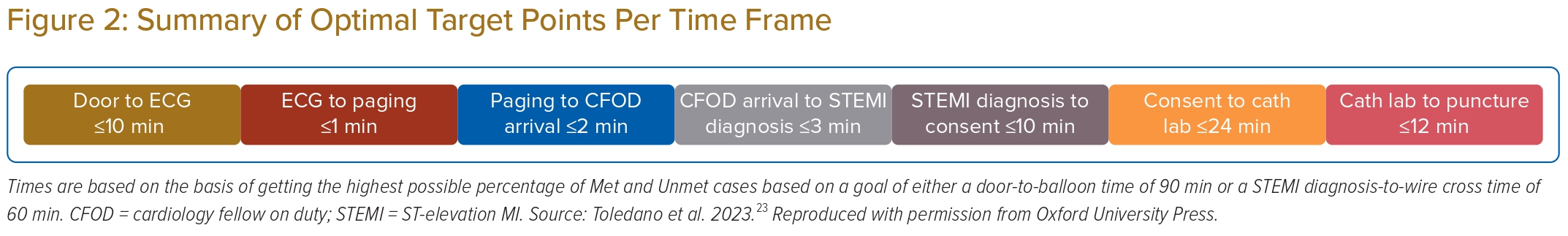
Table 1 summarises the patients’ clinical profiles, time of arrival, and a comparison of time frames contributing to the DTB. The average age of the patients was 55.34 ± 12.88 years, with a higher proportion of men (84.96%) than women. Most patients arrived during office hours (60.18%). The time of arrival did not differ significantly between the Met and Unmet groups (p=0.127). There were no significant differences in door to ECG time (median 11 minutes; p=0.071) and paging to CFOD arrival time (median 2 minutes; p=0.529) between the Met and Unmet groups. However, the Unmet group had a significantly longer ECG to paging time (median 2 minutes [IQR 1–11 minutes] versus 1 minute [IQR 0–3 minutes]; p≤0.034) and CFOD arrival to STEMI diagnosis time (median 3 minutes [IQR 1–4 minutes] versus 1 minute [IQR 0–2 minutes]; p=0.008) than the Met group.
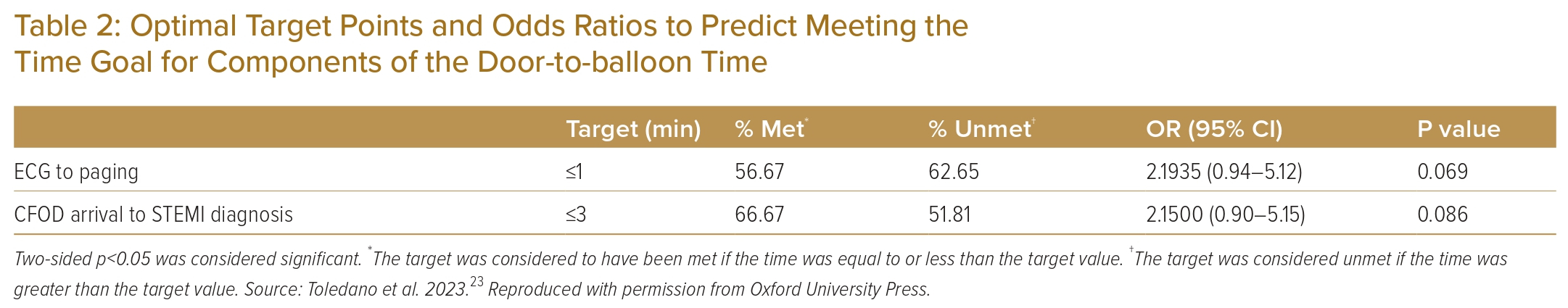
The optimal target for the ECG to paging time is ≤1 minute, with 56.67% in the met group achieving this target and 62.65% in the Unmet group having an ECG to paging time >1 minute. Participants with an ECG to paging time ≤1 minute were twice as likely to meet the DTB time goal than participants with an ECG to paging time >1 minute (OR 2.19; p=0.069), but this was not statistically significant.
For CFOD arrival to STEMI diagnosis, the target point is ≤3 minutes, with 66.67% in the Met group achieving this target and 51.81% in the Unmet group having a CFOD arrival to STEMI diagnosis time >3 minutes. Participants with a CFOD arrival to STEMI diagnosis time ≤3 minutes were twofold more likely to meet the DTB time goal than participants with a CFOD arrival to STEMI diagnosis time >3 minutes (OR 2.15; p=0.086), but this was not statistically significant (Table 2).
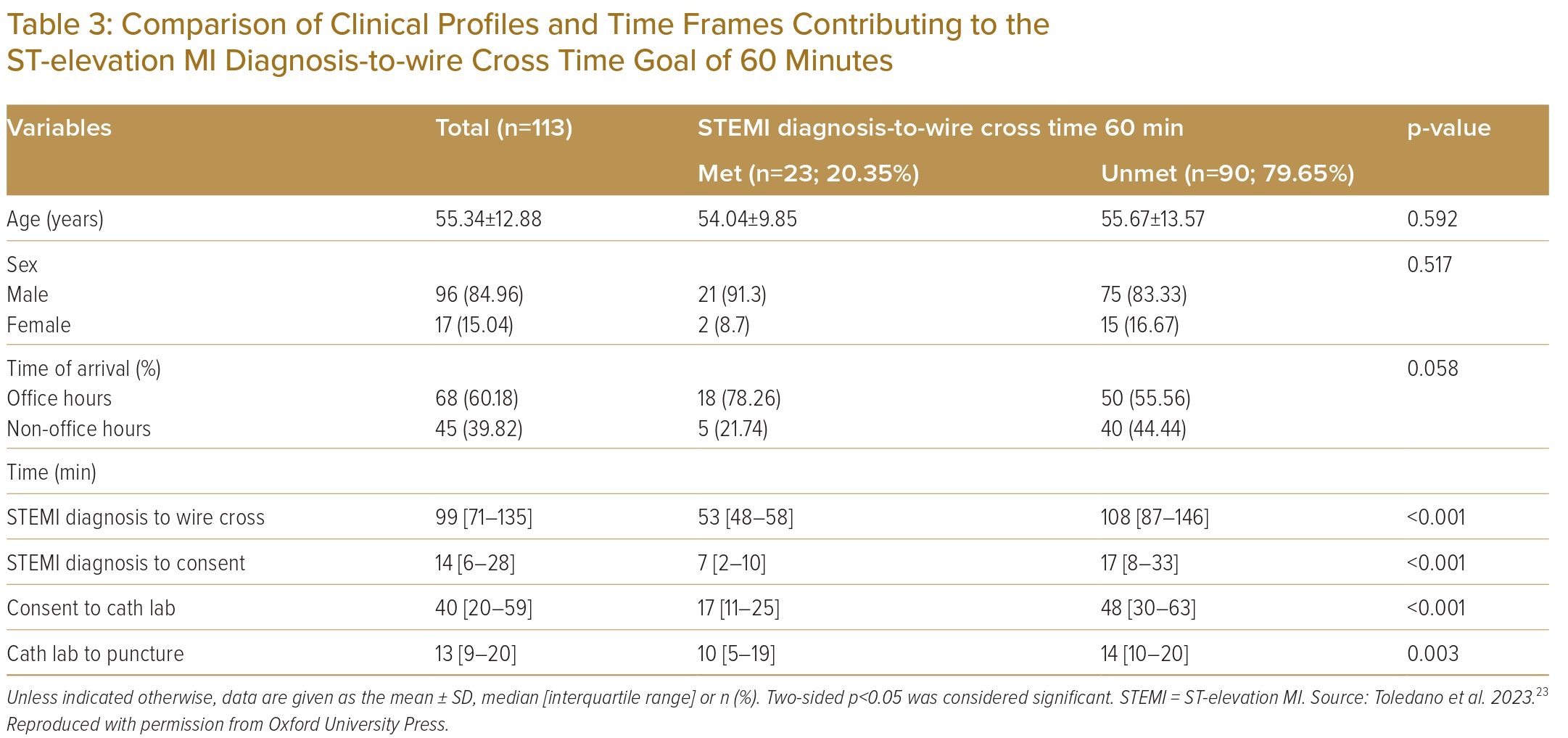
A higher percentage (79.65%) of patients did not meet the STEMI diagnosis-to-wire cross goal of 60 minutes. The clinical profile of these patients, their time of arrival and time frames contributing to the STEMI diagnosis-to-wire cross goal are summarised in Table 3. The time of arrival between the Met and Unmet groups was not significantly different (p=0.0587). The Unmet group had significantly longer times for STEMI diagnosis to wire cross (median 108 minutes [IQR 87–146 minutes] versus 53 minutes [IQR 48–58 minutes]; p≤0.001), STEMI diagnosis to consent (median 17 minutes [IQR 8–33 minutes] versus 7 minutes [IQR 2–10 minutes]; p≤0.001), consent to cath lab (median 48 minutes [IQR 30–63 minutes] versus 17 minutes [IQR 11–25 minutes]; p≤0.001) and cath lab to puncture (median 14 minutes [IQR 10–20 minutes] versus 10 minutes [IQR 5–19 minutes]; p=0.003) than the Met group.
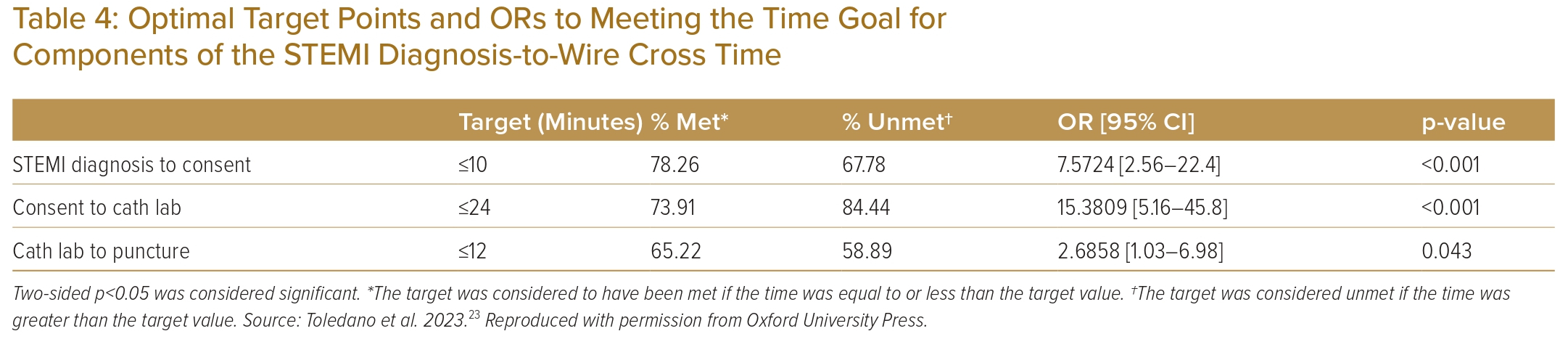
The optimal target for CFOD diagnosis to consent time is ≤10 minutes, with 78.26% of patients in the Met group achieving this target and 67.78% of patients in the Unmet group exceeding the 10-minute threshold. Participants with a CFOD diagnosis to consent time ≤10 minutes were seven times more likely to meet the STEMI diagnosis-to-wire cross time goal than those with a CFOD diagnosis to consent time >10 minutes (OR 7.57; p≤0.001). Similarly, the optimal target for the consent to cath lab time is ≤24 minutes, with 73.91% of patients in the Met group meeting this target and 84.44% of patients in the Unmet group surpassing the 24-minute threshold. Participants with a consent to cath lab time ≤24 minutes were 15 times more likely to meet the STEMI diagnosis-to-wire cross time goal compared to those with a consent to cath lab time >24 minutes (OR 15.38; p≤0.001). For cath lab to puncture time, the target is ≤12 minutes, with 65.22% of patients in the Met group achieving this target and 58.89% of patients in the Unmet group exceeding the 12-minute threshold. Participants with a cath lab to puncture time ≤12 minutes were three times more likely to meet the STEMI diagnosis-to-wire cross time goal than those with a cath lab to puncture time >12 minutes (OR 2.68; p≤0.043; Table 4).
Discussion
In the Philippines, the impact of the COVID-19 pandemic became evident during the first community quarantine in March 2020, with intermittent lockdowns continuing until 2021. To ensure a comprehensive representation of our STEMI response programme and hospital system, we selected an equal duration of 15 months before and during the pandemic. The Medical City hospital is situated in Pasig City with a land area of 48.46 km2 and serves a population of more than 800,000 residents. International studies have indicated a decline in the number of STEMI cases and delays in time to reperfusion during the pandemic, attributed to various factors such as patient-related, hospital system, and procedural delays.11,12 However, the present study did not directly compare time frames before and during the pandemic.
Based on personal observations, the additional time required to don protective gear and implement stringent hospital infection control policies partly accounts for the low percentage of patients meeting the DTB time and STEMI diagnosis-to-wire cross goals. These findings are consistent with reports from the Singapore Western STEMI network, which also reported delayed DTB times and increased in-hospital mortality during the COVID-19 pandemic.13 Similarly, Bainey et al. highlighted that emergency department evaluations were prolonged due to additional screening for COVID-19 and challenges in distinguishing STEMI from other conditions affecting troponin release. Additionally, the transfer of patients from the ER to the cath lab is complicated by the risk of staff exposure and delays associated with preparing personal protective equipment.14 This observation also reflects the shortage of available physicians, nurses and auxiliary personnel.15 Contrary to findings from a multicentre study, the time of patient arrival during office and non-office hours did not significantly contribute to delays.16
The door to ECG time is utilised to determine eligibility for reperfusion therapy. Based on our study, the optimal target point is 9 minutes, which aligns with the established maximum target delay of 10 minutes. Achieving this target has been shown to provide benefits of faster diagnosis, timely initiation of reperfusion therapy and improved clinical outcomes.17 The ECG to paging signal, initiated by ER residents, is triggered by symptoms of MI or ECG findings. The optimal target point is within 1 minute; the considerable number of patients from non-COVID-19 and COVID-19 areas seen by ER residents and atypical ECG patterns may account for the significant delay seen in this step and for the false-positive activations.18
No significant delay was observed from paging to CFOD arrival. The importance of CFODs prioritising a STEMI call above any other obligations was exemplified by achieving the optimal target point of ≤2 minutes. However, there was a significant delay in the CFOD arrival to STEMI diagnosis time, which was likely caused by initially non-diagnostic 12L ECG results and the necessity for serial ECG monitoring to confirm a STEMI diagnosis. A significant delay was also observed in the time from CFOD diagnosis to obtaining consent for emergency PCI. This process is complex and involves the CFOD providing clear information about the risks and benefits of the procedure, addressing concerns, encouraging questions and involving the patient or their relatives.19 Patients or their relatives are expected to make a decision within a short amount of time, and difficulties in retaining information and financial constraints are major concerns.
Additionally, there is a high prevalence of uninsured or underinsured patients in developing countries like the Philippines. Payment issues are notorious for causing delays in obtaining consent, particularly in low- to middle-income countries rather than high-income countries.20 The use of multimedia in delivering information and plans to alleviate the expenses by the Philippines government may help achieve the optimal target point of ≤10 minutes. The longest delay was observed from consent to transfer to the cath lab, which required coordination between the ER and cath lab nurses, as well as the transport team, consisting of an ER resident, CFOD, auxiliary personnel and a pulmonology therapist if the patient was intubated or post-cardiac arrest. A swift and seamless transition and the implantation of a transport protocol for such patients may be necessary to meet the optimal target point of ≤24 minutes.
Lastly, the cath lab to puncture delay may be attributed to the late arrival of the IC consultant. In such cases, the responsibility falls on the IC fellow to initiate the procedure and meet the goal of ≤12 minutes. While having an in-house IC consultant would be the ideal set-up, it may not be feasible in our setting. Therefore, recommendations include increasing the number of IC consultants on call and ensuring their close proximity to the hospital.
Based on the optimal target point obtained, the maximum allotted time for the hospital system to achieve the DTB and STEMI diagnosis-to-wire cross goals is 62 and 46 minutes, respectively (Figure 2). This allows the operator a 14- to 28-minute window to wire or balloon the infarct-related artery. While not common, there are reports of procedural delays in cases involving tortuous vessels and anomalous origins of coronary arteries.21,22 The goal of achieving revascularisation as quickly as possible is fundamental knowledge for all those involved in STEMI management. Although unforeseen circumstances may arise and cause delays, having an optimal target point based on past experiences provides a concrete measure for each member involved within each time frame to achieve the time goals that improve patient care.
Recommendation
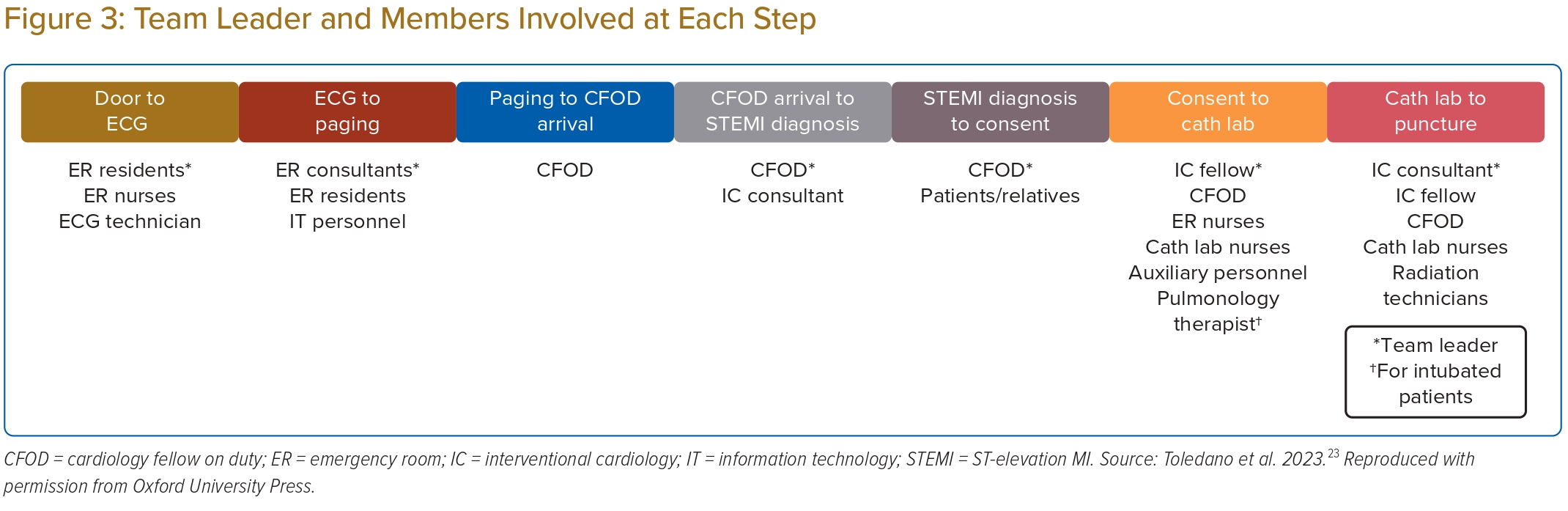
In the real-time scenario of the current system at The Medical City hospital, STEMI patients typically arrive via private car. Establishing an emergency medical system will help reduce STEMI delays by enabling immediate prehospital diagnosis, obtaining consent and facilitating direct transfer to the cath lab. At The Medical City hospital, we recommend assigning a team leader for each time frame to monitor and supervise the members involved, ensuring they meet these target points and ultimately achieve the STEMI time goals (Figure 3).
Limitations
This is a small, single-centre, retrospective study conducted in a private institution. To substantiate our findings and enable generalization, a large, multicentre, prospective study involving private and government institutions in the Philippines is needed. Additionally, in-hospital morbidity and mortality outcomes are necessary to demonstrate the benefits of achieving the optimal target points for each time frame and reducing STEMI delays.
Conclusion
This single-centre retrospective study identified system delays and target points to provide concrete objectives that may increase the chances of achieving DTB and STEMI diagnosis-to-wire cross goals. The most significant delays of our STEMI programme occurred while obtaining consent for emergency PCI and transferring patients to the cath lab. 
Clinical Perspective
- Prompt revascularisation is crucial for the treatment of ST-elevation MI.
- Hospital delays should be identified and audited to reduce ischaemic time.
- Certain issues and challenges are present in developing countries with limited resources during the COVID-19 pandemic.
- Setting optimal target points for each time frame may increase the chances of achieving the door-to-balloon and ST-elevation MI diagnosis-to-wire cross goals.