Globally, ischaemic heart disease (IHD) remains a main cause of mortality, amounting to more than 9 million deaths in 2016 alone.1 The burden of IHD is particularly prevalent in low- to middle-income countries, where the rates of mortality and risk for IHD among those aged <60 years are reported to be high.1,2 In Malaysia, IHD is the major cause of national mortality, contributing to 15.6% of all deaths in 2018.3 The 2019 National Cardiovascular Disease Database for acute coronary syndrome (ACS) revealed a total of 21,327 patients being admitted for ACS between 2016 and 2017; 44.6% of which were because of ST-elevation MI (STEMI), 28.0% for non-STEMI (NSTEMI) and 27.4% for unstable angina.4
Data describing the common characteristics of patients presenting with chest pain to emergency departments (EDs) remain sparse in Malaysia and regionally. A study from an Ecuadorian rural hospital revealed 2.8% of patients aged <60 years and 5.4% of those aged >60 years presented to the ED with chest pain, whereas a study from Pakistan (involving seven major EDs) revealed a rate of approximately 7%.5,6
It is important for ED clinicians to triage patients presenting with chest pain as either cardiac, likely cardiac or non-cardiac in nature.7 Furthermore, decisions are needed to identify patients who would benefit from hospitalisation versus those who can be safely discharged.8 Failure to do so effectively may lead to not only financial and institutional consequences (i.e. exit blocks), but also to compromised care for those requiring immediate clinical management. Patients with MI who are prematurely discharged have a doubled risk of mortality compared with those who are hospitalised.8,9 Therefore, rapid and accurate diagnosis, followed by thoughtful risk stratification of ACS in the ED is paramount.10
Cardiac troponins (cTn) I and T remain the conventional biomarkers used to detect myocardial injury, risk-stratify patients suspected of ACS, and subsequently diagnose MI.11 Recent guidelines have recommended using high-sensitivity cardiac troponin (hs-cTn) assays to triage patients with suspected ACS.11–14 According to the International Federation of Clinical Chemistry (IFCC) and Laboratory Medicine Task Force on Clinical Applications of Bio-Markers, for an assay to be defined as high-sensitivity, two analytical criteria need to be fulfilled: analytical imprecision (% coefficient of variation) at the 99th percentile upper reference limit (URL) should be ≤10%; and highly-sensitive assays should measure cTn at or above the assay’s limit of detection in ≥50% of healthy subjects.15,16 Despite strong recommendations in adopting routine use of hs-cTn, less sensitive point-of-care testing (POCT) is often a preferred choice in majority of hospitals due to rapid access of results without on the need for central laboratory involvement.
The aim of this evidence-based expert consensus is to provide guidance for healthcare professionals in understanding the role of hs-cTn, specifically its level of sensitivity and specificity, as well as its practical application in the ED setting, particularly in resource-limited centres. Discussions will be based on case scenarios throughout this guide.
Methods
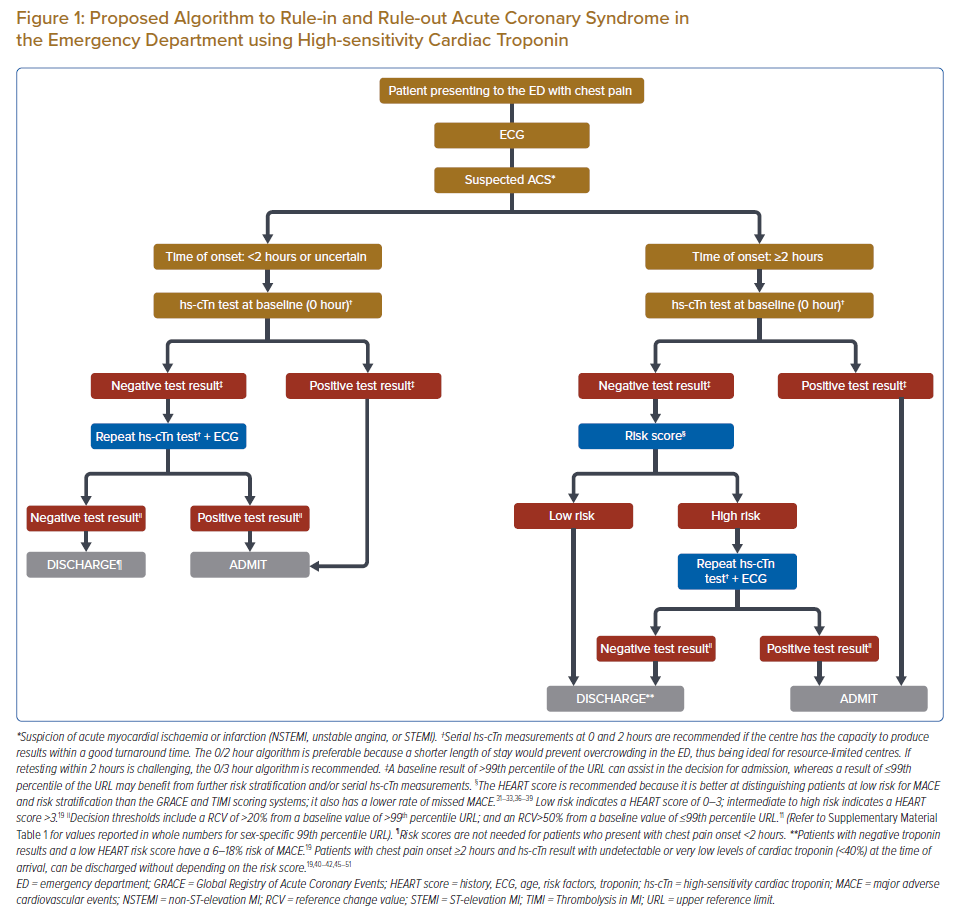
An expert panel with clinical and research expertise in the diagnosis and treatment of ACS was convened. This consisted of cardiologists, family medicine physicians, emergency medicine physicians and chemical pathologists from public, university and private healthcare settings in Malaysia. Three meetings were held between August 2019 and February 2020, with an agenda to formulate recommendations on hs-cTn testing. These recommendations were based on a comprehensive review of the existing literature using MEDLINE and Embase databases, alongside individual clinical experience. Level of evidence was based on an adaptation of the Levels of Evidence by the Oxford Centre for Evidence-Based Medicine. During these meetings, participating members identified problems, created frameworks and suggested input statements, which were used in subsequent meetings to develop this paper. After incorporating all feedback, a unanimous agreement was reached for final evidenced-based decisions on an algorithm (Figure 1) and consensus recommendations for the use of hs-cTn to diagnose ACS in the ED.
Results
Assessing for Acute Coronary Syndrome in the Emergency Department: The Five Steps
To address the gaps in current ACS diagnosis in the ED, particularly in resource-limited centres, the panel agreed on a five-step approach using hs-cTn. These steps are:
- Obtaining patient history and determining symptom onset.
- Performing a clinical examination, ECG and echocardiography.
- Performing initial hs-cTn testing.
- Performing risk stratification.
- Determining diagnosis.
These recommendations are based on the need to fully use hs-cTn in ensuring prompt diagnosis of patients with possible ACS and prompt discharge of patients at lower risk of ACS or other serious conditions. The panel’s five-step approach is incorporated in the proposed algorithm for ruling in or ruling out ACS in the ED (Figure 1) and these steps are elaborated in the subsequent paragraphs.
Step 1: Patient History and Symptom Onset
By obtaining a comprehensive patient history, physicians can identify possible serious and life-threatening causes for chest pain and exclude less critical differentials. Essential components include information on the nature of the pain itself (i.e. site, onset, characteristics, radiation, duration, alleviating and/or exacerbating factors and severity). The presence of associated symptoms such as shortness of breath, palpitations, ankle oedema, orthopnoea and paroxysmal nocturnal dyspnoea is also pertinent. Detailed descriptions of pain and discomfort can also help exclude other non-cardiac causes of pain.
It is recommended that physicians establish the exact onset, duration and pattern of symptoms by allowing patients to describe the symptoms themselves (i.e. avoiding coaching). This will not only improve patient recall, but also allow for more accurate diagnosis, which subsequently leads to better patient care.17,18 It is also important to establish cardiovascular risk factors, such as diabetes, hypertension, hyperlipidaemia, a family history of premature heart disease, smoking and a sedentary lifestyle. However, it should be noted that women can present with atypical symptoms and hence under-diagnosis is common in this cohort who are further under-represented in clinical trials. This is also similar in patients aged >75 years. Thus, additional attention should be paid to these two cohorts.7
Acute chest ‘pain’ or ‘discomfort’ may encompass a tightness, heaviness, pressure, fullness, or squeezing sensation that starts gradually and worsens, or does not improve with resting, lying down, drinking water or other measures. Patients may present a few hours – or even up to several days – after the onset of chest pain. As the timing of the onset is important in determining the role of hs-cTn testing, the panel recommends a cut-off time of 2 hours. There is evidence that physicians can safely identify patients who only need a single troponin level based on symptom onset, which justifies the recommendations on incorporating this element of history taking. However, the authors acknowledge that setting a cut-off time point is often challenging as in practice patients are sometimes unable to determine the exact onset of their symptoms, although efforts should be made by clinicians to estimate the timing.19–21
Step 2: Physical Examination, ECG and Bedside Echocardiography
Physical examination remains key in identifying the patient’s general condition and determining the level of illness severity. Physicians should look for signs of flushing, discomfort or sweating and review the patient’s vital signs upon arrival to the ED. Discrepancies in pulse or blood pressure should alert to the possibility of aortic dissection. An elevated jugular venous pressure, presence of gallop rhythm, leg oedema and basal crackles may indicate presence of congestive cardiac failure. One key diagnostic tool for MI is the ECG.22 However, we would remind readers that the ECG should be performed concurrently with the initial triage of the patient in ED, and possibly even before a thorough history taking is performed. This is to help identify a STEMI prior to other steps in this pathway, which would alter the management pathway significantly. Furthermore, additional ECG leads such as leads V3R, V4R and V7 to V9, are recommended if on-going ischaemia is suspected when standard leads are inconclusive to help exclude right-sided and posterior MI.
Bedside transthoracic echocardiography has also proven to be a useful tool in the initial management of acute chest pain. It allows clinicians to identify left ventricular regional wall motion abnormalities suggestive of underlying ischaemic pathology, and helps to identify important differentials such as an acute pulmonary embolism and aortic dissection. It is also important to highlight the need for adequate training in performing and interpreting results from echocardiography before including it into routine clinical practice.7,23
Step 3: Initial High-sensitivity Cardiac Troponin Testing
Initial hs-cTn testing should be conducted as soon as possible if ACS is suspected.12 The hs-cTn assay’s diagnostic troponin concentration cut-off for MI is the 99th percentile value of the reference population. Levels of cTn above the 99th percentile upper reference limit (URL) indicate myocardial injury.11 A multicentre study to examine the diagnostic accuracy of cTn assays found hs-cTn assays to have a negative predictive value (NPV) of 99%.24 As the various cTn assays have distinct biological and analytical characteristics, the clinical decision limits to suggest possible MI for each assay would be different.25 Different populations may also have different URLs, and the use of cohort-specific URLs would further improve the diagnosis of ACS.26–28 Supplementary Material Table 1 shows variable 99th percentile URLs for assays based on studies in Malaysia and two other developing countries.
Major organisations, such as the European Society of Cardiology (ESC), American College of Cardiology (ACC), American Heart Association, World Heart Federation and IFCC, have recognised lower values of hs-cTn assay URLs for women than for men in their recommendations .11,29 With sex-specific thresholds, women are five times more likely to be identified with myocardial injury than men.30 Supplementary Material Table 1 includes sex-specific 99th percentile URLs for the assays showing a lower URL for women. However, an Asia-Pacific consensus has otherwise underscored the routine need for sex-based cut-off values, as little was to be gained in clinical outcome when patients were reclassified.13 It should be noted that criteria on hs-cTn assays differed between studies versus that recommended by the IFCC. Laboratories should, therefore, establish their own hs-cTn reference values based on the assays available.
Readers should also note several other causes for raised hs-cTn levels beyond myocardial injury, such as chronic kidney disease (CKD), that should be taken into consideration during interpretation of the test. Given the lack of data in the Malaysian population, it should be acknowledged that both the positive predictive value and NPV of tests, including hs-cTn, is dependent upon the population of interest. A handful of studies have since be published describing the accuracy and also limitations of hs-cTn, which is a topic beyond the scope of this paper.12,13,27
Step 4: Risk Stratification
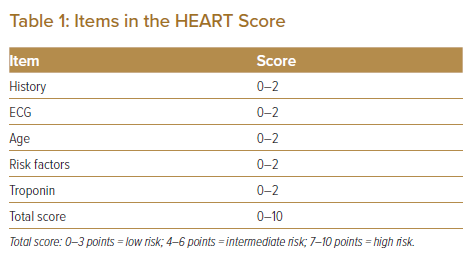
Risk assessment tools such as the HEART score should be incorporated to distinguish between patients who are at low, intermediate, or high risk for ACS-related outcomes (Table 1).31 The HEART score was first developed in 2008 as a rapid risk-stratification tool to determine the short-term risk of major adverse cardiovascular events (MACE) in patients with chest pain and has been extensively validated for use in the ED. Although the original study included patients with an identified acute MI (AMI), the HEART score is generally not used to assist with the management of patients with ACS, but to risk stratify patients who have a negative work-up in the ED who may need further testing or observation.31,32 By excluding the patient identified with an AMI from the ED cohort, this substantially changes the estimated risk for MACE in an ED population.33 Clinicians should note that scores between 0–3 indicate low risk, while scores ≥3 indicate higher risk, but this may differ depending on the patient population.20,34
The HEART score has been shown to be a better risk tool for patients with low risk for MACE and for risk stratification versus Global Registry of Acute Coronary Events and Thrombolysis in Myocardial Infarction scoring, with its lower rate of missed MACE (Supplementary Material Table 2).31,32,35–39 When performed together, patients with negative troponin results and low HEART scores have a 6–18% risk of MACE.19
It should be noted that there is also evidence that the combination of both troponin and risk stratification can be more reliable than a troponin level alone, although the evidence is not as substantial.40,41 Clinicians should be encouraged to use clinical judgement to identify such patients based on history, the patient’s HEART score and ECG findings. Clinicians should bear in mind that risk scores are not recommended in patients presenting within 2 hours of chest pain onset. Such patients, if accompanied by a negative hs-cTn result with undetectable or at very low levels of hs-cTn at the time of arrival, can be discharged without depending on risk scoring.19,42–51
Step 5: Diagnosis
During this stage, serial measurements of hs-cTn may be necessary. Myocardial injury may be acute, evident by a newly detected dynamic rise and/or fall of cTn values above the 99th percentile URL, or chronic in the setting of persistently elevated levels.11 Serial hs-cTn measurements at 0 and 2 hours from the first blood test are recommended if the laboratory is able to produce results within the expected turnaround time. The 0/2 hour algorithm is ideal as shorter length of stay within ED would prevent overcrowding especially in resource-limited centres. Studies have shown that with hs-cTn, MI can be excluded within 2 hours of presentation in the ED.52 If retesting within 2 hours is challenging, the 0/3 hour algorithm is recommended.
The reference change value (RCV) is defined as the critical difference that must be exceeded between two sequential results for a significant (or true) change to occur. It is used to determine whether a significant change between two serial troponin values from the same cTn assay is demonstrated. This is calculated using the following formula:
Reference change value = 2 h value − 0 h value
The RCV considers both the biological and analytical variation of hs-cTn.53 For a baseline value of ≤99th percentile URL, an RCV of >50% is recommended as the decision threshold.54,55 For a baseline value of >99th percentile URL, an RCV >20% is suggested as the decision threshold.10 When the RCV is high, ACS is likely (high specificity, lower sensitivity for MI), whereas when the RCV is low, ACS becomes unlikely (higher sensitivity, lower specificity for MI).56 The use of an absolute RCV (in ng/l), which is assay dependent is preferable to relative RCV (in %) because it gives a varying set of criteria depending on the baseline value, hence maintaining sensitivity.11,57,58 For the sake of brevity, this consensus paper has not included the cut-off values for various high-sensitivity troponin assays, which are readily available online.58–61
Discussion
The proposed algorithm remains to be validated in larger populations, but nevertheless provides a useful foundation to improve ED triaging of patients presenting with acute chest pain. Patients presenting to the ED with chest pain who are deemed likely to have ACS should be admitted to an intensive care unit (ICU) or a non-ICU monitored setting, depending on their level of risk as evaluated in the ED. Patients presenting to the ED with chest pain who are unlikely to have ACS may be discharged and evaluated as outpatients.
Subsequent investigations, such as an echocardiogram, stress test, nuclear perfusion study and MRI, should be considered.62 Low-risk patients discharged with follow-up evaluation through a primary care physician and/or cardiologist have a significantly reduced risk of death or MI at 1 year.63 Patients unlikely to suffer from ACS may also benefit from referrals to other specialties to identify alternative causes for chest pain.59
It should be noted that data to suggest a significant reduction in mortality remain scarce at present from such practice. However, there have been several publications highlighting the benefit of incorporating high-sensitivity troponin testing in helping to identify low-risk patients, allowing for deferral of early non-invasive cardiac testing safely while simultaneously decongesting the ED. This may lead to better patient care in the acute setting as it allows for redirection of resources and services to those who truly require them.64–67
Our expert consensus document was developed following difficulty in incorporating recommendations from international guidelines, such as those of the ESC, ACC and Asian Pacific Society of Cardiology. We provide several hypothetical scenarios below to better demonstrate the role of the proposed algorithm.
Rule-out Protocol for Acute Coronary Syndrome with High-sensitivity Cardiac Troponin
Recommendation 1: Chest pain onset of <2 hours, with an initial hs-cTn ≤99th percentile URL followed by second hs-cTn with RCV of <50% may rule out ACS.
Case scenario 1: A 58-year-old man presented to the ED with central chest pain, which occurred <2 hours earlier. He described the pain as pricking and lasting 10 minutes with no associated symptoms. He had a history of diabetes, hypertension and hypercholesterolaemia, and smoked regularly. On physical assessment, he was pain free. His vital signs and clinical examination were unremarkable. His ECG revealed sinus rhythm with no ischaemic changes.
This man presented with a short duration chest pain, which occurred <2 hours earlier. He has several cardiovascular risk factors. Although his ECG was normal, an initial hs-cTn test, followed by a second test 2 hours after the initial blood test, is recommended. If both the hs-cTn test results are normal, MI can be safely ruled out. The hs-cTn algorithms have high sensitivity and high NPV, and further investigations to rule out MI are unnecessary. The patient can be discharged from the ED and safely evaluated as an outpatient. An alternative approach, outside the proposed algorithm, would be to perform a second hs-cTn test and to observe if the results are similarly ≤99th percentile URL (as opposed to observing RCV), which can appear much safer and clinicians should be encouraged to use the clinical gestalt to identify such patients based on history, the patient’s HEART score and ECG findings. Furthermore, early follow-up outpatient assessment by a cardiologist or a general physician should also be considered.
Recommendation 2: Chest pain onset of ≥2 hours before presentation, low HEART score, and hs-cTn ≤99th percentile URL may rule out ACS.
Case scenario 2: A 50-year-old man with underlying hypertension complained of central chest pain, which occurred >2 hours prior to hospital arrival. The pain lasted for 10 minutes and was associated with mild breathlessness. He denied any palpitations, sweating or loss of consciousness. On physical assessment he was alert and not in distress. His pain score was 2/10. His vital signs and clinical examination were unremarkable. His ECG revealed sinus rhythm with no ischaemic changes.
This 50-year-old man presented to the ED with chest pain >2 hours prior. His ECG was normal. The first hs-cTn test was negative (≤99th percentile URL). Despite a history of hypertension, his cardiovascular risk remains low based on his HEART score of 3. A second hs-cTn test is not deemed necessary and the patient can be discharged with subsequent outpatient follow-up, as described by Wassie et al. where safe discharge based on history and a single troponin testing was considered safe.21
Recommendation 3: Chest pain onset of ≥2 hours, and hs-cTn ≤99th percentile URL followed by second hs-cTn with RCV of <50% even with a high HEART score may rule out ACS.
Case scenario 3: A 65-year-old woman with underlying hypertension, diabetes and dyslipidaemia presented with chest heaviness associated with breathlessness, which occurred 4 hours earlier. The pain occurred when she was climbing up a staircase and resolved with rest. At the time of physical assessment, she was pain free. Her vital signs and clinical examination were unremarkable. Her ECG revealed sinus rhythm changes consistent with left ventricular hypertrophy.
This woman complained of chest pain on assessment. The ECG revealed sinus rhythm with left ventricular hypertrophy changes. The first hs-cTn was negative (≤99th percentile URL). As the patient had multiple cardiovascular risk factors (hypertension, diabetes and dyslipidaemia), her HEART score was 6 (moderate risk). For this patient, hs-cTn test should be repeated 2 hours from initial testing. Following a second test that shows no significant change from baseline (RCV ≤50%) the patient can be discharged with subsequent follow-up within an outpatient setting.
However, similar to case scenario 1, an alternative approach could be undertaken, which can appear much safer. Again, clinicians should be encouraged to use clinical gestalt to identify such patients based on history, HEART score and ECG findings, alongside early outpatient follow-up. Even in the absence of positive results through repeated hs-cTn testing, it would be reasonable for clinicians to observe the patient within a medical assessment unit or observation bay which has since become a common adjunct in most EDs in Malaysia. This may allow for medical optimisation of cardiovascular risk factors including blood pressure and glycaemic control acutely, prior to discharging the patient for outpatient follow-up.
Rule-in Protocol for Acute Coronary Syndrome with High-sensitivity Cardiac Troponin
Recommendation 4: Chest pain onset of <2 hours before presentation and initial hs-cTn >99th percentile URL may rule in ACS.
Case scenario 4: A 46-year-old man presented to the ED with central chest pain, which occurred an hour earlier. He had no history of diabetes, hypertension, or hypercholesterolaemia but smoked regularly. His ECG showed poor R wave progression. His renal profile was normal on laboratory testing.
The patient had short-duration chest pain with cardiovascular risk factors. Based on the ECG finding, coronary artery disease was suspected. An initial hs-cTn test followed by a second test (2 hours from presentation) was recommended. If the first hs-cTn test was elevated, the patient should be referred to a cardiologist or responsible physician. A second hs-cTn test is not necessary. The patient was admitted and treated for NSTEMI with dual antiplatelet therapy and low-molecular-weight heparin (LMWH).
Case scenario 5: A 65-year-old man with hypertension, dyslipidaemia, stage 3 CKD and diabetes complained of left-sided chest discomfort, which occurred 30 minutes before arrival to the hospital. The pain lasted for 20 minutes and was associated with mild sweating. On physical assessment, he was alert and had minimal pain. A coronary angiogram conducted 8 years ago was normal. His pain score was 3/10. His vital signs and clinical examination were unremarkable. His ECG revealed sinus rhythm with T-wave inversions in lead III and aVF. His renal profile was deranged, with an estimated glomerular filtration rate of 45 ml/min/1.73 m2.
This patient presented to the ED, with complaints of chest pain that occurred <2 hours earlier. His clinical history indicated high suspicion for acute coronary syndrome. Serial ECGs taken 15 minutes apart, revealed non-specific repolarisation disturbance. The first hs-cTn test result was positive (>99th percentile URL). The patient was admitted and treated for NSTEMI with dual antiplatelets and LMWH.
A caveat to consider would be that the patient has concomitant CKD, as this may lead to elevation in hs-cTn levels, both in presence or absence of myocardial injury. However, the expert panel believes that patient suffering from CKD, especially those in the later stages (i.e. stage 4 and 5) are of a particularly higher risk and would benefit from closer evaluation as an inpatient whenever feasible. Inpatient review should incorporate serial hs-cTn testing to better assess risk and allow closer monitoring for acute cardiopulmonary decompensation in this otherwise fragile group of patients. This is also largely supported by evidence that even among patients with renal dysfunction without ACS, raised troponin levels are observed in about 40%, often not because of reduced renal clearance, but instead via myocardial injury through uraemia, increased left ventricular pressure, hypotension, microvascular dysfunction and anaemia.13
We would recommend further reading on differences in definition of MI, differentiating both Type 1 and 2 MI as well, which is beyond the scope of this consensus paper.11
Recommendation 5: Chest pain onset of <2 hours before presentation and initial hs-cTn ≤99th percentile URL followed by second hs-cTn with RCV of >50% may rule in ACS.
Case scenario 6: A 35-year-old woman with hypertension and diabetes complained of left-sided chest discomfort, which occurred an hour prior to arrival to the hospital. The pain lasted for 15 minutes and was associated with mild dyspnoea. This was the patient’s first episode, and it was brought on by moderate exertion. On physical assessment, she was alert and pain free. Her vital signs and clinical examination were unremarkable. Her ECG revealed sinus rhythm with no ischaemic changes.
This patient presented to the ED complaining of chest pain that occurred within 2 hours. Her clinical history indicates moderate suspicion for coronary artery disease. Initial ECG showed non-specific repolarisation disturbance. The initial hs-cTn test was negative (≤99th percentile URL) and her HEART score was 3, indicating low risk. The patient was observed for further chest pain, while remaining pain free.
Serial ECGs, taken 15 minutes apart, revealed no progressive changes. However, the second hs-cTn test result (conducted 2 hours after the first test) showed an RCV of >50% from baseline value. The patient was admitted and treated for NSTEMI with dual antiplatelets and LMWH. There was also emphasis on better blood pressure and glycaemic control, with regular close monitoring of her capillary blood glucose levels, as diabetic ketoacidosis remains a possible life-threatening differential.
Recommendation 6: Chest pain onset of ≥2 hours before presentation and initial hs-cTn >99th percentile URL may rule in ACS.
Case scenario 7: A 64-year-old man presented to the ED with central chest pain, which occurred 4 hours earlier. He had history of diabetes, hypertension and hypercholesterolaemia and smoked regularly. His ECG was normal.
This patient presented with chest pain that occurred beyond 2 hours from presentation. He had multiple cardiovascular risk factors. His ECG was normal. An initial hs-cTn test, followed by a second test (2 hours from initial testing) was performed and returned positive (>99th percentile URL). The patient should be referred to a cardiologist or responsible physician. In this case, a second hs-cTn is unnecessary.
Case scenario 8: A 36-year-old male smoker complained of retrosternal chest pain, which occurred 2 hours prior to hospital arrival. The pain lasted for an hour and was associated with sweating, nausea and vomiting. He required parenteral opioid and isosorbide dinitrate infusion to control the pain. On physical assessment he appeared anxious and his pain score was 6/10. His vital signs and clinical examination were unremarkable. His ECG revealed sinus rhythm with ST depression at leads l and V2–V6, and T-wave inversions at II, III and aVF.
This patient presented to the ED complaining of chest pain that occurred more than 2 hours earlier. Based on ECG results and his prolonged chest pain (lasted for 1 hour) and accompanying symptoms, ACS was suspected. As the first hs-cTn test result was positive (>99th percentile URL), he was admitted for NSTEMI and treated with dual antiplatelets and LMWH. As the patient is in a high-risk category, risk scoring and a second hs-cTn were not necessary.
Recommendation 7: Chest pain of unknown onset and initial hs-cTn ≤99th percentile URL followed by second hs-cTn with RCV of ≤50% may rule in ACS.
Case scenario 9: A 68-year-old male smoker with hypertension and dyslipidaemia developed central chest pain, which radiated to both shoulders 3 hours prior. The pain lasted for 20 minutes before it gradually subsided. He vomited once. On physical assessment, his pain score was 3/10. His vital signs were unremarkable. Examination revealed a third heart sound with bibasal crepitations. His ECG revealed sinus rhythm with ST-segment depression at leads II, III and aVF, and T-wave inversions at V4–V6, I and aVL.
This patient presented to the ED complaining of chest pain that occurred prior to his arrival. The time of onset of chest pain was unknown. He had multiple cardiovascular risk factors. His ECG revealed sinus rhythm with significant ST deviation. Based on ECG and clinical history, ACS was highly suspected. An initial hs-cTn test was conducted upon arrival, but results were negative (≤99th percentile URL). The HEART score was 8, indicating high risk for cardiovascular disease. Although a second hs-cTn test repeated 2 hours after the initial test demonstrated an RCV ≤50%, the patient was still admitted for observation and inpatient work-up for ischaemic heart disease.
The reason for introducing this case scenario is to remind clinicians that guidelines and recommendations should never replace clinical gestalt. Despite two negative hs-cTn tests, the patient’s clinical history, HEART score and ECG were worrying enough to support a decision for observation and further investigation, ideally as an inpatient. This may include a transthoracic echocardiogram to look for new regional wall motion abnormalities, serial hs-cTn testing, coronary artery assessment via CT imaging or imaging for evidence of ischaemia via cardiac MRI or nuclear myocardial perfusion imaging.
The Use of Other Cardiac Troponin Assays in the Emergency Department
Although conventional cTn tests have high diagnostic accuracy, hs-cTn testing has been shown to be more sensitive.60,68,69 A meta-analysis revealed that hs-cTn had significantly greater sensitivity (0.884 versus 0.749; p<0.001) and NPV (0.964 versus 0.935; p<0.001) compared to the conventional assay in patients with chest pain.60 However, when hs-cTn testing is unavailable or inaccessible, POCT may be a reasonable alternative to diagnose ACS in the ED.12 These tests have a short turnaround time, making them suitable in EDs where there is overcrowding or poor access to laboratories.70,71 However, it should be noted that many POCT cTn assays have lower sensitivity, diagnostic accuracy and NPV than central laboratory tests.63,64,72–74 One study showed that a POCT cTn assay had 68% sensitivity compared to a hs-cTn assay, which had a 98% sensitivity for excluding MI.70 The NPV was 95% for POCT troponin compared to 98% for hs-cTn.70 Additionally, POCT has high rates of under-diagnosis. In one study, the POCT for troponin missed 29% of patients with acute MI or unstable angina.75 Therefore, extreme caution is required when using POCT troponin to rule out ACS in the ED.
Non-ischaemic Myocardial Injuries
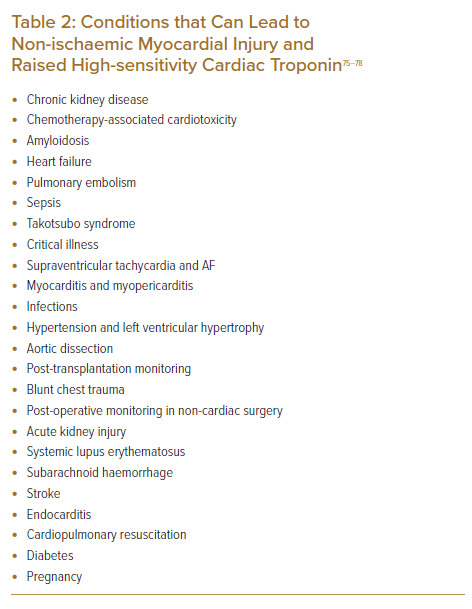
In cases with low pre-test probability for myocardial ischaemia, efforts should be made to identify alternative causes for symptoms. Physicians should be familiar with various conditions where non-ischaemic myocardial injury could occur and cause raised troponin levels (Table 2) to avoid premature diagnosis of ACS, which then leads to inappropriate cascading of investigations and interventions.76–78 However, raised troponins are often useful for prognosis even in such cases, and can guide management. Information from other diagnostic modalities such as transoesophageal echocardiography, late gadolinium enhancement in cardiac MRI, CT coronary angiogram and – when necessary – the conventional coronary angiogram, should be used in conjunction with serial cTn measurements to establish a diagnosis.
Late Presentation in Patients with NSTEMI
It should be noted that in patients presenting beyond 12 hours with an initial elevated hs-cTn, care should be taken in the interpretation of differences in values between subsequent results. Patients with adjudicated NSTEMI with less acute presentations, and those with longer ischaemic times, are more likely to present closer to their peak hs-cTn value. Subsequent values may experience reduction or plateau, which can at times provide false reassurance to clinicians away from the diagnosis of NSTEMI. This is important because small changes in cardiac enzyme levels are common in patients with NSTEMI who remain at substantial risk for mortality.79 A way to circumvent this is by identifying high-risk features linked to ACS. Although this remains beyond the scope of this manuscript, we provide the necessary references for the perusal of readers.80
Conclusion
Our expert consensus provides a structured approach to using hs-cTn in the ED. It remains the only one to date produced by a group of Malaysian experts to help guide local healthcare providers in dealing with patients presenting with acute chest pain. A local consensus statement was felt necessary as it would incorporate essential information based on local availability of diagnostic and therapeutic modalities. Having a scenario-guided consensus statement would also supplement existing recommendations on the use of high-sensitive troponin testing in the ED setting, while enforcing the need for practicing clinicians to use their clinical acumen when in doubt, to avoid test-related issues.
Click here to view Supplementary Material.
Clinical Perspective
- High-sensitivity cardiac troponin assays are currently recommended to help triage patients with suspected acute coronary syndrome.
- However, despite strong recommendations in adopting high-sensitivity cardiac troponin, less sensitive rapid assays are often a preferred choice in majority of hospitals because of rapid results without the need for central laboratory involvement.
- Our expert consensus provides guidance for healthcare professionals in understanding the role of high-sensitivity cardiac troponin, specifically its level of sensitivity and specificity as well as its practical application in the emergency department setting, particularly in resource-limited centres.