Risk stratification and prognostication is an important step for the management of acute MI (AMI). The Thrombolysis in MI (TIMI) and Global Registry of Acute Coronary Events (GRACE) risk scores have been demonstrated to have reasonably good discriminatory value, including in Asian populations.1 Other predictors, including reduced left ventricular ejection fraction (LVEF) and poor recovery of LVEF after AMI, have also been long recognised in risk stratification for patients with AMI.2,3
N-terminal pro brain natriuretic peptide (NT-proBNP) is an established biomarker for the diagnosis of heart failure. However, its role for risk stratification in AMI remains debatable. The 2020 European Society of Cardiology guideline on the management of acute coronary syndrome (ACS) states that measurement of brain natriuretic peptide (BNP) or NT-proBNP plasma concentrations should be considered to obtain prognostic information (class IIa, level of evidence B).4
While there are established cut-off values for the association between GRACE risk scores and in-hospital mortality, there is no clear cut-off value for NT-proBNP to guide risk stratification in patients with AMI. Moreover, most studies have been conducted in white populations and remain to be validated in Asian populations. In light of differences in genetic background and environmental factors, our study team decided to conduct this study in a local Asian, multi-ethnic population. The study sought to evaluate the NT-proBNP cut-off value for predicting 1-year mortality in patients with AMI and to compare this with other available risk scores.
Study Objectives
The primary objective of the study was to explore the cut-off value of NT-proBNP to predict 1-year all-cause mortality in AMI patients. The secondary objective was to compare the prognostic value of NT-proBNP with the TIMI and GRACE risk scores and with LVEF.
Methods
This multicentre, prospective observational study was conducted in one cardiology referral centre (Sarawak Heart Centre) and four non-cardiology general hospitals (Sibu Hospital, Miri Hospital, Bintulu Hospital and Kapit Hospital). Informed consent was obtained from each patient. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the Malaysia Ministry of Health Medical Research and Ethics Committee (NMRR-16-1195-31525).
Patients and Eligibility Criteria
AMI was defined according to the fourth universal definition of MI.5 The exclusion criteria included age <18 years or >80 years, haemodynamic instability on presentation (cardiogenic shock, septicaemic shock, anaphylactic shock), high bleeding risk (unexplained anaemia, haematocrit <25%, history of blood transfusion within the 14 days prior to screening or active life-threatening bleeding), end-stage renal failure receiving dialysis, active cancer with life expectancy <1 year, pregnancy or being unable to provide informed consent.
Study Procedure
An NT-proBNP point-of-care (POC) test was performed within 24 hours from the diagnosis of AMI. Plasma NT-proBNP level was measured with the Alere Triage NT-proBNP POC test. The analytic range extends from 20 to 35,000 pg/ml, with a range of precision (% coefficient of variation) of 8.4–16.4%.
Approximately 3 ml of blood was drawn by direct venipuncture and collected in an ethylenediaminetetraacetic acid tube. Whole blood was taken within 24 hours of diagnosis with an MI, irrespective of whether this was before or after percutaneous coronary intervention (PCI). The result was available in approximately 20 minutes.
TIMI Risk Score, GRACE Risk Score and Left Ventricular Ejection Fraction Measurement
For patients with non-ST-elevation MI (NSTEMI), TIMI risk score was assessed with the variables of age ≥65 years, three or more traditional risk factors for vascular disease, known coronary stenosis ≥50%, presence of ≥0.5 mm ST-segment deviation on admission ECG, two or more episodes of angina in the last 24 hours, positive biomarkers and the use of aspirin in the last 7 days.6 For patients with ST-elevation MI (STEMI), TIMI risk score was assessed with the variables of age, diabetes, hypertension or angina, systolic blood pressure <100 mmHg, heart rate >100 BPM, Killip class ≥2, weight >67 kg, anterior ST-elevation or left branch bundle block ECG and time to treatment of >4 hours.7 A TIMI risk score of ≥3 was used as the cut-off for comparison with NT-proBNP in predicting all-cause mortality.
The GRACE risk score was calculated based on the GRACE 2.0 ACS risk calculator using the online calculator or iPhone/Android app.8 Four continuous variables (age, systolic blood pressure, pulse rate, serum creatinine); three binary variables (cardiac arrest at admission, elevated cardiac biomarkers, ST-segment deviation); and one categorical variable (Killip class at presentation) were assessed. A GRACE risk score of ≥140 was used as the cut-off for comparison with NT-proBNP in predicting all-cause mortality.
LVEF was measured by transthoracic echocardiogram using EPIQ7 ultrasound system (Philips) with X5-1 transducer. 2D echocardiogram images were obtained from apical four- and two-chamber views. Images were acquired using harmonic imaging at a frame rate of 40–80 frames per second. Manual tracing of left ventricle endocardial borders at end diastole and end systole was performed. Modified biplane Simpson’s rule was used to calculate left ventricular end-diastolic volume, left ventricular end-systolic volume and LVEF. An LVEF of <40% was used as the cut-off for comparison with NT-proBNP in predicting all-cause mortality.
Follow-up and Study Endpoints
All patients received the standard of care for AMI in hospital. Patients were followed up via telephone interviews at the end of 1, 6 and 12 months after discharge. Serial echocardiogram assessments were arranged at 6 and 12 months after discharge. The study endpoint was all-cause mortality at 1 year. The Youden index was used to select the optimum cut-offs from the receiver operating characteristic (ROC) curve. The cut-off value was selected if the sensitivity was >80%. If the sensitivity of the cut-off value selected by the Youden index was <80%, then the nearest cut-off value with a sensitivity of ≥80% was selected.
Statistical Analysis
Numerical variables in this study were presented as mean ± SD and median (interquartile range [IQR]). Categorical variables were presented with counts (percentages). For univariate analyses of numerical variables, the independent sample t-test was used for parametric data and Mann–Whitney test in nonparametric variables. Survival analyses were generated using the Kaplan–Meier method, and the differences between the groups were assessed via the log-rank test. A Cox proportional hazard model was used to calculate the crude and adjusted HR with corresponding 95% CI. All analyses in this study were performed using the SPSS software package (Version 20, IBM). A value of p<0.05 was considered significant.
Results
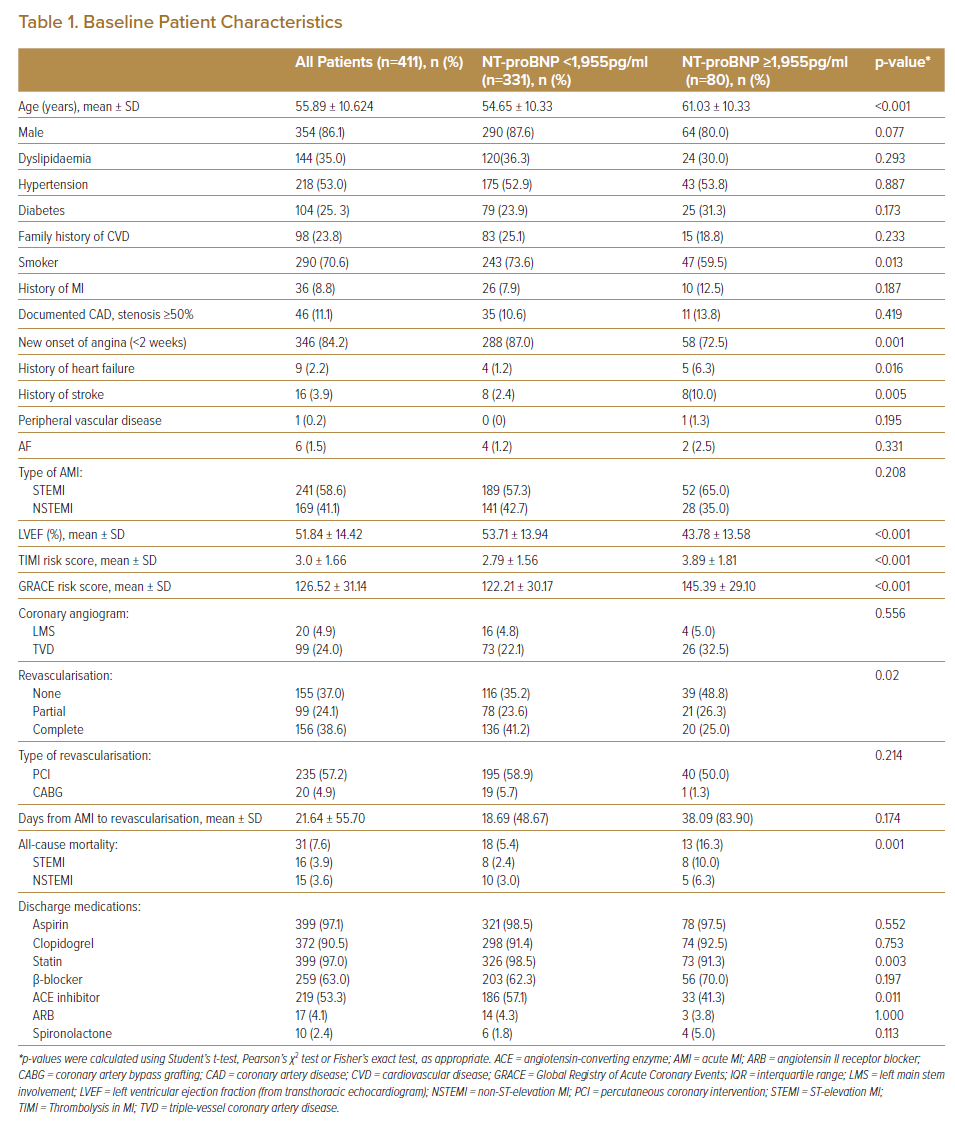
A total of 411 patients who presented with AMI to the emergency department between 1 August 2016 and 6 October 2017 were recruited to the study. Mean age was 55.89 ± 10.62 years. In total, 70.6% of patients had a history of smoking, 84.2% had new onset of angina, and 25.3% had diabetes. A total of 58.6% of the patients presented with STEMI. Overall, 74.3% of STEMI patients received fibrinolytic therapy. Of the 411 patients, 255 (62.7%) underwent partial revascularisation (revascularisation to the infarct-related arteries) or complete revascularisation within 1 year. Of the revascularisations, 235 (92.2%) used PCI while the remaining 20 (7.8%) used coronary artery bypass grafting (CABG). The mean duration from index event to revascularisation (PCI or CABG) was 21.6 ± 55.7 days (Table 1).
Primary Outcome
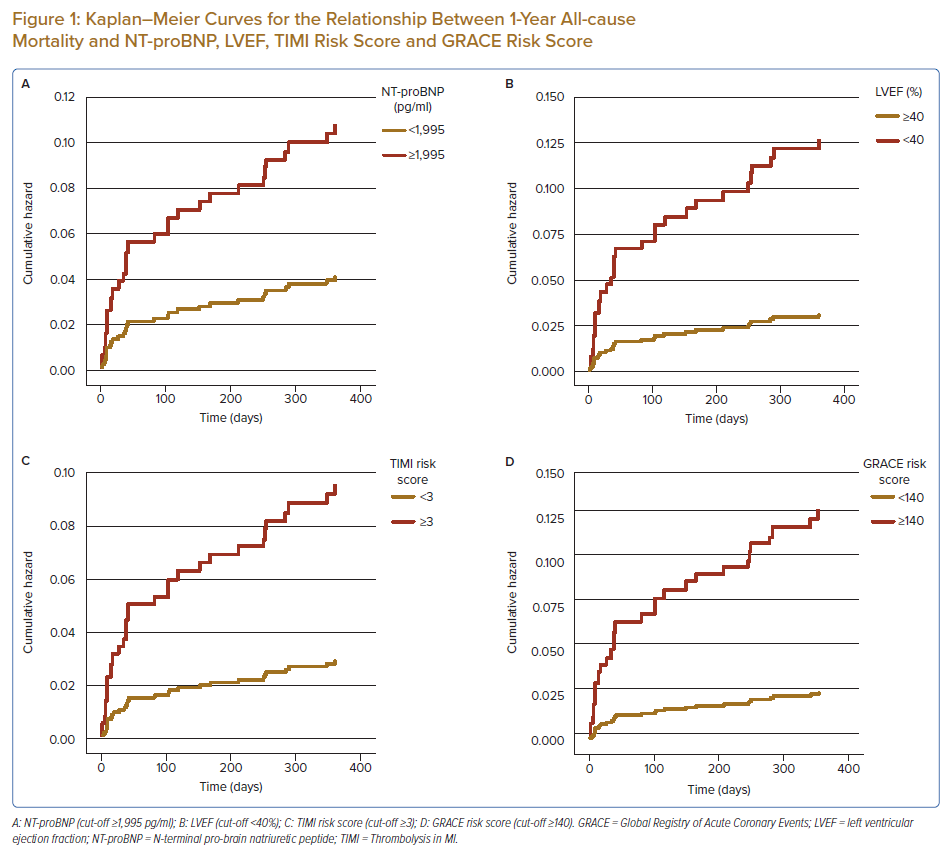
One-year all-cause mortality occurred in 31 (7.6%) of 411 patients. Twenty-four patients (5.9%) had cardiac-related death and seven were due to non-cardiac causes. The median (IQR) duration from the index AMI event to the primary outcome was 40 (9–211) days. The associations between all-cause mortality at 1 year and NT-proBNP level, TIMI risk score, GRACE risk score and LVEF are described in the subsequent sections (Figure 1).
NT-proBNP
Plasma NT-proBNP level was not normally distributed in the study population. The median (IQR) NT-proBNP level was 655 pg/ml (463–4,940 pg/ml; range 20–32,900 pg/ml). The NT-proBNP level was not statistically different between patients presenting with NSTEMI compared with STEMI (1,883.26 ± 4,723.41 pg/ml versus 1,536.75 ± 2,232.86 pg/ml; p=0.322). More patients in the group with STEMI had single- or double-vessel disease (75.9 versus 64.5%), while more patients in the NSTEMI group had triple vessel disease or left main stem involvement (35.5% versus 24.1%, p=0.012).
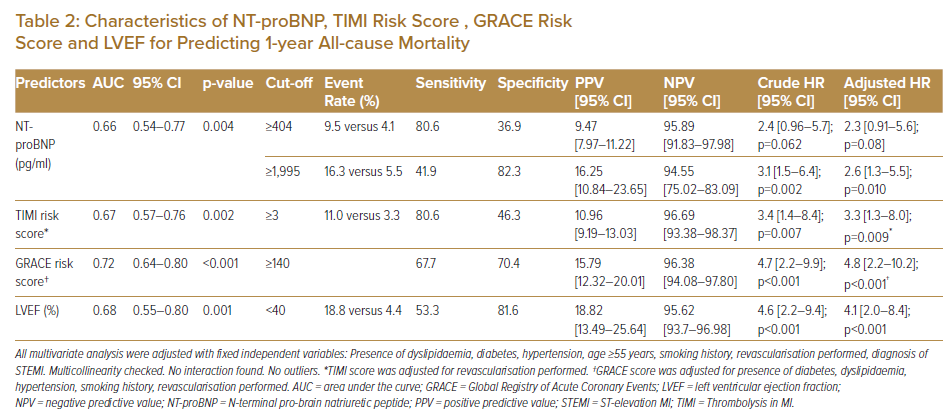
The ROC curve of the plasma NT-proBNP level for all-cause mortality had an area under the curve (AUC) of 0.66 (95% CI [0.54–0.77]; p=0.004). The first plasma NT-proBNP cut-off level with a sensitivity of 80.6% and specificity of 36.9% was selected based on the Youden index. Plasma NT-proBNP ≥404 pg/ml (frequency of 64.5%) was not associated with all-cause mortality (HR 2.4; 95% CI [0.96–5.7]; p=0.062). The second plasma NT-proBNP level with a specificity of >80% (specificity 82.3%, sensitivity 41.9%) was selected using the Youden index. Plasma NT-proBNP level ≥1,995 ng/ml (frequency of 19.5%) was significantly associated with all-cause mortality (HR 3.1; 95% CI [1.5–6.4]; p=0.002).
Multivariate analysis showed that NT-proBNP level ≥1,995 pg/ml was an independent predictor for all-cause mortality, regardless of the revascularisation status prior to the events (adjusted HR 2.6; 95% CI [1.3–5.5]; p=0.010) (Table 2). This demonstrated that AMI patients with NT-proBNP level ≥1,995 pg/ml on presentation were 2.6 times more likely to have all-cause mortality within 1 year.
There was higher all-cause mortality in the group of patients with NT-proBNP <1,995 pg/ml who had medical therapy compared to those who had revascularisation (11.3 versus 2.3%; p=0.001). In the group of patients with NT-proBNP ≥1,995 pg/ml, there was no significant difference in all-cause mortality between the two groups (20.5 versus 12.2%; p=0.313).
Left Ventricular Ejection Fraction, NT-proBNP and All-cause Mortality at 1 Year
LVEF was not normally distributed. The mean ± SD for LVEF was 51.84 ± 14.42% (range 12.0–88.0%). The ROC curve of the LVEF for all-cause mortality at 1-year had an AUC of 0.68 (95% CI [0.55–0.58]; p=0.001). LVEF of <40% was selected based on the Youden index with a sensitivity of 53.3% and specificity of 81.60%.
Patients with LVEF <40% had a four times increased risk of all-cause mortality at 1 year. (HR 4.6; 95% CI [2.2–9.4]; p<0.001), regardless of revascularisation status (adjusted HR 4.1; 95% CI [2.0–8.4]; p<0.001; Table 2). NT-proBNP level was inversely associated with lower LVEF (r −0.3, p<0.001). There were 86 patients (20.9%) with LVEF <40% upon admission and 55 (13.4%) with LVEF <40% at 1 year.
TIMI Risk Score, GRACE Risk Score, NT-proBNP and All-cause Mortality at 1 Year
The TIMI risk score ranged from 0 to 9 (mean ± SD 3.0 ± 1.7), and 224 (55.9%) patients had TIMI ≥3. The ROC curve of the TIMI risk score for all-cause mortality at 1-year had an AUC of 0.67 (95% CI [0.57–0.76]; p=0.002). Patients with TIMI ≥3 were three times more likely to have all-cause mortality at 1 year (HR 3.4; 95% CI [1.4–8.4]; p=0.007) regardless of the revascularisation status (adjusted HR 3.3; 95% CI [1.3–8.0]; p=0.009).
The GRACE risk score ranged from 52 to 238 (mean ± SD 126.5 ± 31.1). A total of 133 (32.4%) of patients had a GRACE risk score ≥140. The ROC curve of the GRACE risk score for all-cause mortality at 1-year had an AUC of 0.72 (95% CI [0.64–0.80]; p<0.001). A GRACE risk score ≥140 was significantly associated with all-cause mortality at 1 year (HR 4.7; 95% CI [2.2–9.9]; p<0.001), regardless of the revascularisation status (adjusted HR 4.8; 95% CI [2.2–10.2]; p<0.001). NT-proBNP level was significantly correlated with both TIMI risk score (r = 0.3, p<0.001) and GRACE risk score (r = 0.3, p<0.001).
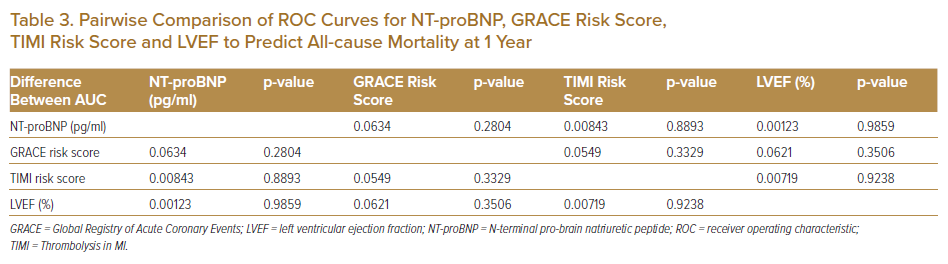
The ROC curves for NT-proBNP, LVEF, TIMI risk score and GRACE risk score were compared using pairwise comparison. There was no significant difference among the four ROC curves in predicting all-cause mortality at 1 year (Table 3 and Figure 2).9
Discussion
Our study showed that higher NT-proBNP level measured within 24 hours of presentation of AMI was significantly associated with higher all-cause mortality at 1 year. NT-proBNP as a biomarker has the potential to serve as a reasonably good screening tool. A cut-off NT-proBNP level ≥1,995 pg/ml was independently associated with all-cause mortality at 1 year. Patients with acute MI and NT-proBNP level ≥1,995 pg/ml were 2.6 times more likely to have all-cause mortality at 1 year. Using the Youden index, NT-proBNP level ≥404 pg/ml had good sensitivity (80.6%) and negative predictive value (95.89%) to predict all-cause mortality at 1 year. However, when adjusted for revascularisation status, it was not significantly associated with the primary outcome. NT-proBNP ≥1,995 pg/ml had a specificity of 82.3% and negative predictive value of 94.55% to predict all-cause mortality at 1 year. The association was significant regardless of the revascularisation status.
Considering that higher NT-proBNP level was inversely associated with LVEF and given the fact that 92.2% of the revascularisation in our patients was PCI, in AMI patients with NT-proBNP level ≥1,995 pg/ml, revascularisation with PCI did not improve all-cause mortality. Similarly, medical therapy has comparable all-cause mortality at 1 year to revascularisation with PCI if the NT-proBNP level was ≥1,995 pg/ml.
The EXCEL trial demonstrated that elevated NT-proBNP levels were associated with higher mortality in patients with left main disease who underwent revascularisation, but were not associated with non-fatal major adverse cardiovascular events.10 In a cohort of 6,597 triple vessel coronary artery disease (TVD) patients (CABG, PCI or medical therapy), during a median follow up of 7 years, a higher baseline NT-proBNP level (quartile 4 as cut off; NT-proBNP ≥958.3 pmol/l) was strongly associated with an increased risk of all-cause mortality (adjusted HR 1.12), cardiac death (adjusted HR 1.13) and major adverse cardiac and cerebrovascular events (MACCE; adjusted HR 1.10), p<0.05.
Revascularisation was associated with lower risk of MACCE compared to medical therapy, except for patients in the lowest quartile. The outcomes after PCI versus CABG for revascularisation of left main coronary artery disease may be conditioned by baseline BNP level, with higher BNP levels favouring CABG and lower BNP levels favouring PCI. In our study, 20 (4.9%) and 99 (24%) patients had left main disease and TVD, respectively. There was no significant difference in the severity of coronary artery disease between patients with NT-proBNP level ≥1,995 or <1,995 pg/ml. Therefore, we were not able to find any association with the 1-year all-cause mortality.
Nevertheless, early revascularisation guided by risk stratification with NT-proBNP could be useful in preventing all-cause mortality at 1 year. In our cohort of patients, the median time from the index AMI event to primary outcome was 40 days. However, only 256 (63%) of the patients had partial or complete revascularisation (92% by PCI) with a mean duration from AMI to revascularisation of 21.6 (± 55.7) days.
All-cause mortality rates, particularly due to cardiac-related pathology, could be improved if an invasive strategy could be undertaken early, i.e. within 2 weeks. This can be a challenge in the clinical setting in a developing country like Malaysia. However, early revascularisation guided by NT-proBNP level was not associated with improved clinical outcomes in patients with non-ST elevated ACS.
Further randomised controlled trials are needed to investigate the impact of NT-proBNP guided prognostication in patients with AMI. To date, there is no universal prognostic cut-off level for NT-proBNP. Therefore, the NT-proBNP cut-off value of ≥1,995 pg/ml may guide future randomised controlled trials.
A study by Kontos et al., which measured serial NT-proBNP during admission and at 1-month post MI, demonstrated that patients who had high/high NT-proBNP (high was defined as >450 pg/ml for age ≤50 years, >900 pg/ml for 50–75 years and >1,800 pg/ml for >75 years) were four times more likely to develop all-cause mortality compared to patients who had low/low NT-proBNP at 2-year follow up.11 In a group of NSTEMI patients, Schellings et al. demonstrated that NT-proBNP and GRACE risk score had good predictive value on 1-month mortality (AUC >0.80) compared with TIMI risk score (AUC = 0.61). Adding NT-proBNP to the GRACE risk score did not have any augmented benefit.12 We did not measure serial NT-proBNP in our study and therefore are unable to comment on the prognostic benefit of serial measurement for NT-proBNP level.
The TIMI and GRACE risk scores are the widely used for risk stratification for patients with ACS. However, these risk scores are not well validated in Asian populations. The TIMI risk score has been shown to underestimate 30-day mortality in STEMI patients with diabetes and renal impairment.13 Souza et al. demonstrated that NT-proBNP had predictive value for cardiac-related deaths (C-statistic = 0.78), albeit no evidence that NT-proBNP augmented the prognostic value when combined with GRACE risk score.14 In our study, the TIMI risk score, GRACE risk score and NT-proBNP were shown to have comparable predictive value for 1-year all-cause mortality.
Some researchers have established a cut-off of NT-proBNP for predicting mortality post-ACS.11 However, to date there is no universal cut-off and most studies were conducted in a largely white population. With the emergence of new biomarkers, for instance SGLT2, pentraxin-3 and D-dimer, more studies combining biomarkers as prognostic tools in predicting events post MI have been conducted. In this study, we examined the value of NT-proBNP as an independent prognostic tool.15–18 We found that NT-proBNP was an independent predictor for all-cause mortality in post-MI patients. Future studies could be conducted to combine other potential biomarkers to evaluate if there are added advantages when combined to further improve utility as a screening tool.
Our study has some limitations. Firstly, patients with cardiogenic shock on presentation were excluded from the study. These patients represent the highest risk group in AMI. However, these patients require urgent invasive procedures without further risk stratification or prognostication. Therefore, the authors felt that excluding these group of patients from the study represents the most relevant cohort of patients for prognostication.
Secondly, the baseline characteristics for patients divided by NT-proBNP level ≥1,995 pg/ml were heterogenous. Revascularisation was achieved in 62.3% (92% by PCI), with the mean duration to revascularisation of 22 days. There was a high rate of fibrinolytic therapy, which is explained by longer patient referral or transfer from rural healthcare facilities to the cardiac centre in an urban setting. Outcomes of the study might be different if more revascularisation was done with CABG and the duration to revascularisation shorter. The heterogeneity in revascularisation was reflected in our local practice and may not be generalisable to other settings.
Thirdly, whole blood was taken within 24 hours of MI diagnosis, which could have been before or after revascularisation. Lastly, this study did not include the optimisation of medication therapy during the outpatient visits, which could be a factor determining outcomes. Randomised controlled trials are needed to further evaluate the prognostic value of this cut-off value. Nevertheless, our study provides a guide for future studies using an NT-proBNP cut-off value of ≥1,995 pg/ml.
This study was also conducted in a healthcare system environment where the single cardiology referral centre was located a significant distance from the other four general hospitals, the furthest of which was 800 km by road transfer. Therefore, in such settings – including in Asia – integrating NT-proBNP into the clinical workflow may provide rapid prognostic information to both the immediate healthcare provider and also the referral centre where the AMI patient might continue their care.
A universal cut-off was proposed in this population of patients post MI, STEMI or NSTEMI. NT-proBNP is a biomarker typically associated with the degree of myocardial stretch/stress. Therefore, in a patient presenting with chest pain diagnosed as an AMI early (with an ECG for STEMI or cardiac biomarker of myocardial damage), high NT-proBNP (e.g. >1,995 pg/ml) serves as a clear marker of worse prognosis, thereby improving the risk stratification process. In other words, NT-proBNP at this level independently identifies the patient as being at higher risk for all-cause mortality. The rationale of choosing NT-proBNP over other biomarkers and the usual clinical features of myocardial stretch/strain in AMI is because other features characteristic of its clinical manifestations, such as acute pulmonary oedema, can be difficult to evaluate.
Firstly, in multi-ethnic populations – there are more than 30 distinct ethnic groups in Sarawak and Malaysia – language barriers can be an issue because patients may be most fluent in their own native language. It can be challenging to quickly obtain an accurate and reliable clinical history.
Secondly, a chest radiograph, usually when performed in an A-P projection with a portable X-ray system in the emergency department setting, occasionally produces images that are difficult to interpret accurately. Thirdly, direct imaging of the heart such as portable echocardiography to determine left ventricular function and areas of new regional wall motion abnormality, is not universally available in the majority of hospitals in Malaysia, nor in hospitals in similar clinical settings across the Asia-Pacific region.
Therefore, measuring NT-proBNP using a POC system, especially when coupled with a biomarker for acute myocardial injury, provides the attending clinician a rapid tool for objective and quantifiable risk assessment in a patient with an AMI. By doing so, early identification of the patients at the highest risk can enable referral to tertiary centres with greater urgency, or transfer to higher-level-monitored beds at their own centres, both of which are typically in relatively short supply in most hospitals in Malaysia and the wider Asia-Pacific region.
Conclusion
NT-proBNP level ≥1,995 pg/ml measured within 24 hours upon admission for AMI was associated with higher all-cause mortality at 1 year. The predictive value for all-cause mortality was comparable to other risk assessment scores and LVEF. Randomised controlled trials will be needed to validate the usefulness of NT-proBNP for risk stratification in patients with AMI.
Clinical Perspective
- N-terminal pro-brain natriuretic peptide was an independent predictor of all-cause mortality in patients post MI in this study.
- N-terminal pro-brain natriuretic peptide measurement, using a point-of-care system, provides the attending clinician a rapid tool for risk assessment in a patient with an acute MI.
- This facilitates decision making regarding treatment strategy and enables referrals to tertiary centres with greater urgency.