MI with non-obstructive coronary arteries (MINOCA) is an increasingly recognised entity that occurs in 6% of all patients diagnosed with acute MI.1 The Fourth Universal Definition of Myocardial Infarction Expert Consensus Document defines MINOCA as the absence of ≥50% diameter stenosis in a major epicardial coronary vessel identified on coronary angiography.2 Nevertheless, MINOCA should only be considered a working diagnosis and further evaluation should be undertaken to identify the underlying aetiology.3,4
Two meta-analyses on the use of cardiac MRI (CMR) in MINOCA identify myocarditis and true MI as the two most common causes, accounting for one-third and one-fifth of all cases, respectively.1,5 Other aetiologies include takotsubo cardiomyopathy and coronary vasospasm, although no diagnosis is found in up to one-quarter of patients with MINOCA.
Existing literature on MINOCA is largely focused on Western populations. When compared with MI with obstructive coronary artery disease (MICAD), patients with MINOCA are more likely to be women, younger and have fewer traditional cardiovascular risk factors, such as diabetes and hypertension.3 The prognosis of MINOCA is generally more favourable than MICAD, although some studies have demonstrated similar if not poorer outcomes.1,6–15 Moreover, outcomes vary depending on the underlying cause of MINOCA. Dastidar et al. found that cardiomyopathies have the poorest prognosis, with a mortality rate of 15% at 3.5 years, followed by true MI (4%) and myocarditis (2%).16
Previous studies evaluating the prognostic benefit of medical therapy support the use of renin–angiotensin system inhibitors (angiotensin-converting enzyme inhibitors/angiotensin receptor blockers), statins and β-blockers in MINOCA patients. In contrast, antiplatelet therapy has not been found to confer a protective effect against major adverse cardiovascular events (MACE).16–22
The aim of this study was to compare the clinical characteristics and outcomes of MINOCA and MICAD patients in Singapore.
Methods
Study Protocol and Population
The Singapore Cardiovascular Longitudinal Outcomes Database (SingCLOUD) is an integrated national registry of adult patients with cardiovascular disease on follow up with public hospitals and outpatient clinics.23 Patients are identified using the Singapore Cardiac Data Bank, a quality improvement database tracking cardiac interventions and surgery, and heart failure admissions in public hospitals; and discharge diagnoses associated with cardiovascular disease (e.g. MI, acute coronary syndrome) or heart failure based on ICD coding.
Clinical, laboratory, procedural, prescription, outcomes, administrative and financial data are obtained via the Singapore Cardiac Data Bank, participating public healthcare institutions and the Ministry of Health. Data from these sources flow through a Ministry of Health data grid comprising of six data warehouses prior to entering SingCLOUD.
Data collection for this study was performed as part of the approved SingCLOUD protocol (NCT03760705). Baseline data, such as patient characteristics, medical history, laboratory results, electrocardiogram at presentation and medications prescribed at discharge, were obtained from the database.
This study was conducted in accordance with the standards set forth by the National Medical Research Council Institutional Review Boards and Declaration of Helsinki.
We identified 4,124 patients with a first presentation of acute MI who underwent coronary angiography between 1 January 2011 and 31 December 2014. Patients were classified into two groups: MICAD, defined as the presence of ≥50% stenosis in a major epicardial vessel; and MINOCA, defined as <50% stenosis. This was based on the Fourth Universal Definition of Myocardial Infarction Expert Consensus Document.2
Outcomes
Follow-up data were collected up until 31 December 2017 over a mean duration of 4.5 years. The primary endpoints for this study were all-cause mortality and MACE defined as a composite of all-cause mortality, recurrent MI, hospitalisation for heart failure and ischaemic stroke.
Statistical Analysis
Continuous variables are presented as the mean ± standard deviation and compared using the independent samples t-test, while categorical variables are expressed as absolute numbers and frequencies in percentages, and compared using the χ-squared test. The cumulative survival rate was analysed using the Kaplan–Meier estimator and the log-rank test was used to compare outcomes in MINOCA and MICAD patients. The multivariate Cox proportional hazards model was used to assess the impact of various predictors on the primary endpoints and the corresponding HRs and 95% CI were reported. A p-value of <0.05 was significant. All statistical analyses were performed using Stata version 13.1 (StataCorp).
Results
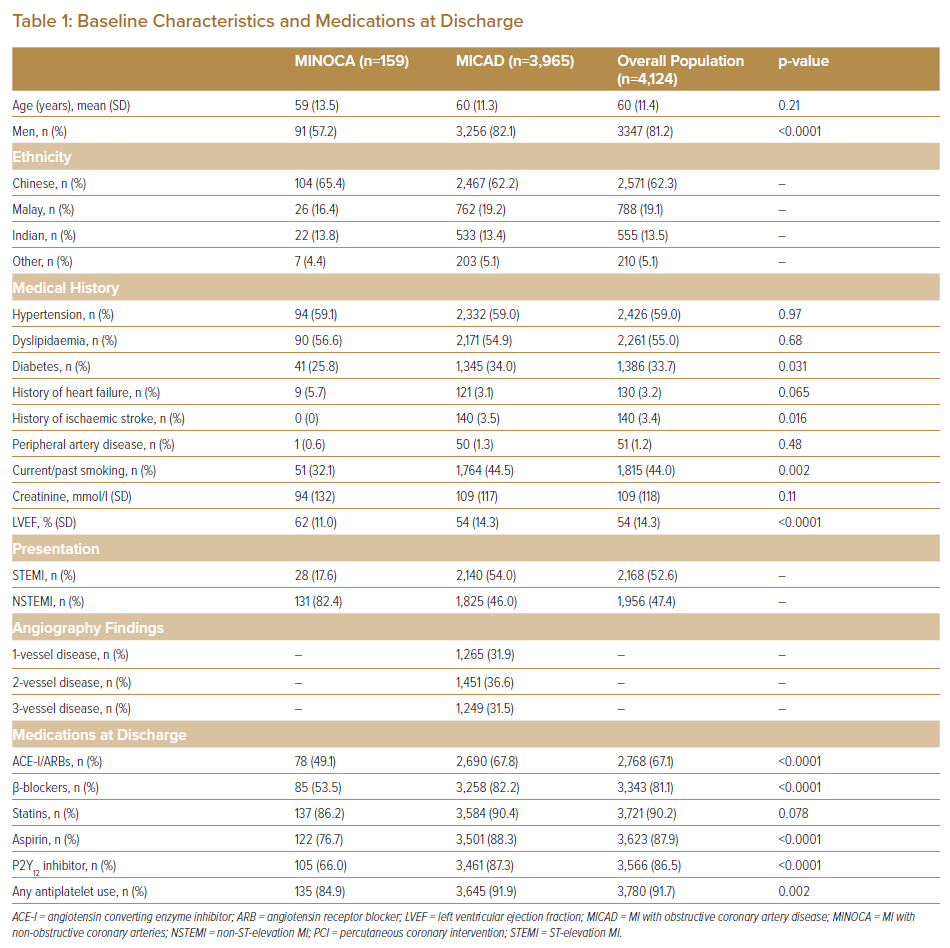
The baseline characteristics of the 4,124 patients included in this study are shown in Table 1. The mean age was 60 years and 81.2% were men. The majority of patients were Chinese (62.3%) followed by Malay (19.1%) and Indian (13.5%), which is consistent with the demographics of Singapore. A total of 159 (3.9%) patients had a diagnosis of MINOCA. Compared with MICAD patients they were more likely be to be women, present with a non-ST-elevation MI, have a higher left ventricular ejection fraction (LVEF) and less likely to have diabetes, previous ischaemic stroke or smoking history. There were no significant differences in the ethnic composition of the two groups. In terms of medications, MICAD patients were more frequently prescribed angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (67.8% versus 49.1%, p<0.0001), β-blockers (82.2% versus 53.5%, p<0.0001) and antiplatelet therapy (91.9% versus 84.9%, p=0.002). The use of statins (90.4% versus 86.2%, p=0.078) was similar in both groups.
Event Rates and Outcomes
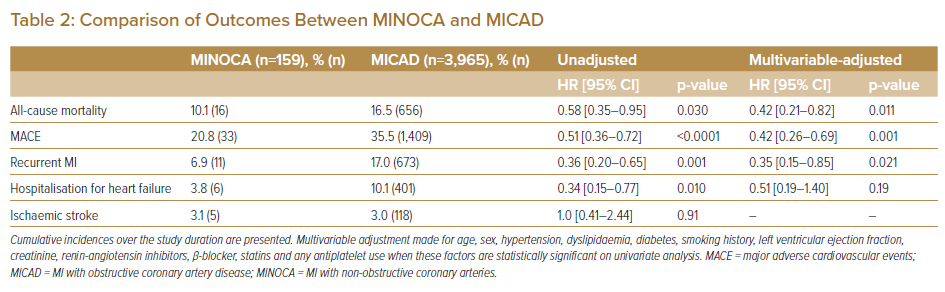
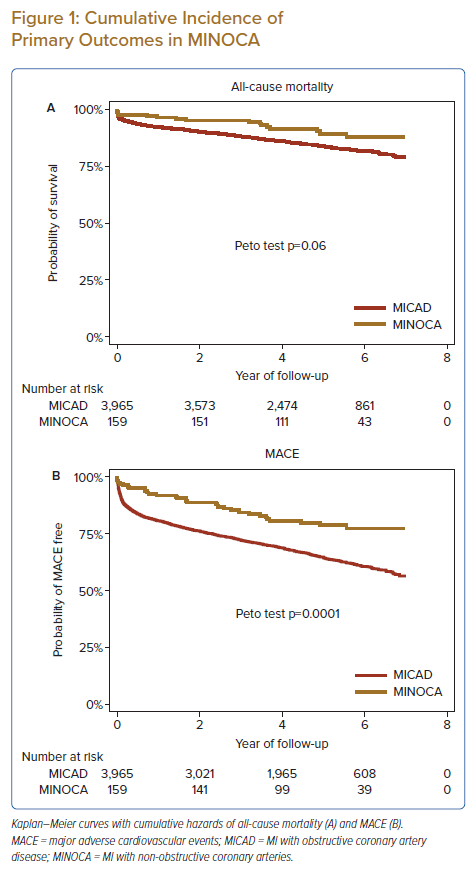
Patients diagnosed with MINOCA experienced a lower incidence of all-cause mortality (10.1% versus 16.5%, p=0.030), overall MACE (20.8% versus 35.5%, p<0.0001), recurrent MI (6.9% versus 17.0%, p=0.001) and hospitalisation for heart failure (3.8% versus 10.1%, p=0.009) compared with MICAD patients over the follow-up period. Using multivariable adjustment, MINOCA patients were at significantly lower risk of all-cause mortality (HR 0.42; 95% CI [0.21–0.82]; p=0.011), MACE (HR 0.42; 95% CI [0.26–0.69]; p=0.001) and recurrent MI (HR 0.35; 95% CI [0.15–0.85]; p=0.021; Table 2). Kaplan–Meier analysis also showed poorer outcomes in the MICAD group (Figure 1).
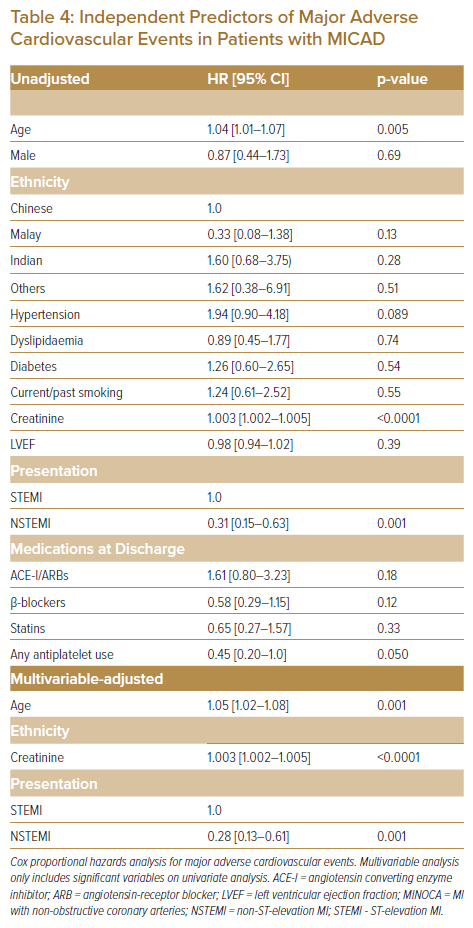
Independent Predictors of Outcomes in MINOCA
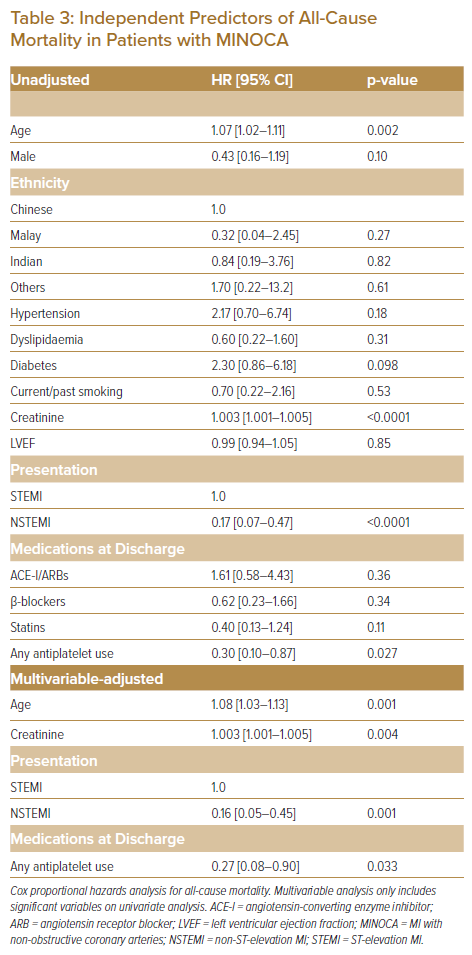
Older age, higher creatinine levels and ST-elevation MI at presentation were identified as independent predictors of all-cause death and MACE using multivariable Cox regression analysis. In addition, the use of antiplatelets (aspirin and/or P2Y12 inhibitors) was associated with a significantly lower risk of all-cause mortality (HR 0.27; 95% CI [0.08–0.90]; p=0.033).
Sex, ethnicity, hypertension, dyslipidaemia, diabetes, smoking status, LVEF, renin–angiotensin inhibitors, β-blockers and statins did not have a significant impact on the primary endpoints. These results are displayed in Tables 3 and 4.
Independent Predictors of Outcomes in MICAD
Supplementary Material Tables 1 and 2 show the independent predictors in MICAD of all-cause mortality and MACE, respectively. On multivariate analysis, older age, hypertension, diabetes, higher creatinine levels, LVEF, statins and antiplatelet use were associated with an increased risk of all-cause death and MACE. The use of renin–angiotensin inhibitors reduced the risk of all-cause mortality, while male sex and ethnicity were independent predictors of MACE.
Discussion
In this nationwide multicentre observational study conducted over a mean follow-up duration of 4.5 years, the prevalence of MINOCA among MI patients was about 4%. Patients with MINOCA had a lesser burden of cardiovascular risk factors and experienced better outcomes than MICAD patients.
The prevalence of MINOCA among patients diagnosed with MI has been estimated to be 6%, which is comparable to the prevalence of 3.9% observed in our cohort.1 Previous studies have shown that MINOCA is associated with female sex, a non-ST-elevation MI presentation, lower rates of smoking and lower prevalence of other traditional cardiovascular risk factors, such as hypertension, dyslipidaemia and diabetes.4 MINOCA patients are also more likely to have a higher post-MI LVEF.16,18 The baseline characteristics of patients with MINOCA in this study were largely consistent with existing literature. Compared with MICAD patients, they were more likely to be female, present with a non-ST-elevation MI, have a higher LVEF and lower rates of diabetes, prior ischaemic stroke and smoking. There were no intergroup differences in ethnic composition.
It is generally accepted that patients with MINOCA have a better prognosis than MICAD patients.1,6–10 A large Medicare study involving more than 276,522 patients found that the rates of all-cause mortality, MACE and rehospitalisation for MI and heart failure at 12 months were lower in MINOCA patients than in MICAD patients, while rehospitalisation for stroke was similar in both groups.11 MINOCA patients in the study also had a 43% lower risk of MACE over 1 year. This is consistent with the results of our study, with MINOCA patients having a lower incidence and risk of all-cause mortality, MACE and recurrent MI. This contrasts with some studies that have reported that MINOCA patients experience similar if not poorer outcomes when compared with patients with MICAD.12–16 This discrepancy likely reflects the heterogeneity of MINOCA, the small (and therefore potentially non-representative) sample size of some previous series, and the influence of variation in underlying aetiologies ranging from true MI and myocarditis to takotsubo cardiomyopathy and coronary vasospasm.1,5 Regardless, the event rate in this group of patients is not insignificant and highlights the importance of secondary prevention.
Patients diagnosed with MINOCA represent an undertreated population, and there are currently no completed randomised controlled trials to date that have investigated secondary prevention medical therapy in MINOCA. Recruitment of adequate sample sizes for controlled trials obviously presents a major challenge. The recent 2020 European Society of Cardiology guidelines recommend performing a CMR in all patients with MINOCA to determine the underlying aetiology and to institute treatment according to the disease-specific guidelines.24 For patients without an established underlying cause, the guidelines recommend treating as per the secondary prevention guidelines for atherosclerotic disease.
However, the management of MINOCA varies widely in clinical practice for various reasons, including accessibility to CMR. It is not uncommon for some physicians to prescribe the same combination of drugs used in atherosclerotic MI for all patients with MINOCA without prior evaluation with CMR. These medications are primarily aimed at plaque stabilisation, reducing atherosclerotic progression and improving endothelial function.25,26 However, MINOCA represents a diverse group of conditions and involves varying pathophysiological processes besides atherosclerosis.1 This challenges the therapeutic basis of using standard MICAD treatment in all MINOCA patients.
Similar to our cohort, prior studies have shown that MINOCA patients were less frequently started on conventional secondary prevention treatments, such as renin–angiotensin system inhibitors, β-blockers and antiplatelets.8,16,18 Several observational studies have suggested a beneficial effect of renin–angiotensin system inhibitors, statins and β-blockers on both short- and long-term outcomes when used in MINOCA patients.16,18,19,22,23 However, these medications did not appear to have a significant prognostic benefit when used in MINOCA patients in our cohort. In contrast, and as expected, renin–angiotensin inhibitors and statins were associated with improved outcomes in our MICAD cohort. Interestingly, the use of antiplatelets in our MINOCA cohort was independently associated with a reduction in all-cause mortality. This stands in contrast with existing literature and may reflect the aetiological heterogeneity of MINOCA.
The ongoing MINOCA-BAT trial is a randomised multinational study investigating the use of β-blockers and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers in MINOCA patients, and represents a crucial first step towards establishing guidelines for secondary prevention in MINOCA (NCT03686696).27 Future trials should also aim to individually identify the underlying aetiology, so as to facilitate tailored medical therapy for each specific condition.
Study Limitations
The limitations of this study are its observational methodology and the small sample size of MINOCA patients, which may not be powered to study the impact of medications on outcomes. In addition, the various exact underlying aetiologies of MINOCA were not established due to a lack of further cardiac evaluation with CMR and other modalities.
Conclusion
While patients with MINOCA had better clinical outcomes compared with MICAD patients, MINOCA is not a benign entity, with about one in five patients experiencing a major adverse cardiovascular event in the long term.
Click here to view Supplementary Material.
Clinical Perspective
- Patients with MINOCA have fewer cardiovascular risk factors and experience better outcomes compared with MICAD patients.
- MINOCA is not a benign entity and is associated with significant adverse cardiovascular events.
- Future studies on MINOCA should incorporate investigations to determine the underlying aetiology and evaluate the impact of medical therapy on each specific condition.