The survival rate of patients with repaired tetralogy of Fallot (TOF) has improved markedly, and most patients reach adulthood. Therefore, residual complications in adulthood have emerged as new problems among these patients. Right ventricular outflow tract obstruction (RVOTO) is one such residual complication, and the number of reoperations for TOF in adulthood has been increasing.1 However, the optimal timing of and indications for reoperation remain controversial. In this report we describe a patient with repaired TOF in whom right heart catheterisation (RHC) with a dobutamine stress test was useful in assessing the dynamics and severity of RVOTO, and determining the treatment strategy.
Case Report
A 32-year-old man presented to Tottori University Hospital with shortness of breath and syncope on exertion. He had been diagnosed with TOF at 1 month of age. At 1 year of age, he had undergone interventricular septal closure and right ventricular outflow tract (RVOT) plasty with a monocusp valved outflow patch (MVOP) at another hospital. Although he had regularly visited the Department of Paediatrics at the same hospital, he had stopped going to the hospital and taking medication at 24 years of age. Eight years later, he developed shortness of breath on exertion. One day, he developed syncope on his way home. He quickly regained consciousness and presented at Tottori University Hospital the next day.
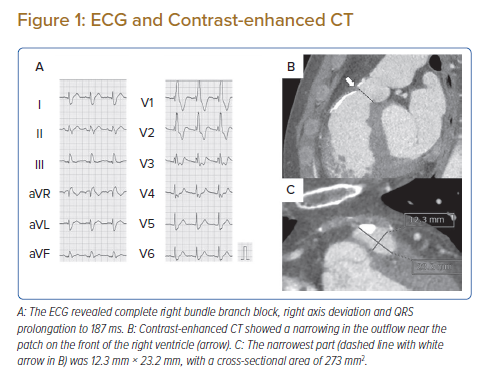
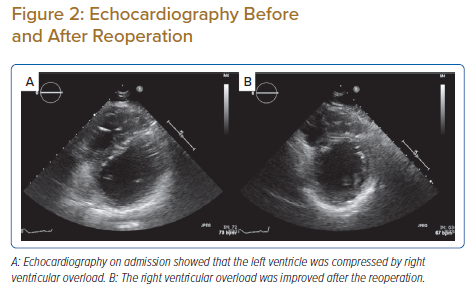
Chest auscultation revealed a systolic murmur (Levine 3/6) from Erb’s point to the second left sternal border. Laboratory tests revealed no obvious abnormalities. The B-Type natriuretic peptide concentration was 7.3 pg/ml. An ECG revealed complete right bundle branch block, right axis deviation and QRS prolongation to 187 ms (Figure 1A). On transthoracic echocardiography, left ventricular (LV) systolic function was normal, and no residual shunt was detected. The estimated systolic right ventricular (RV) pressure at rest was approximately 50 mmHg, and narrowing of the RVOT at the MVOP was suspected although poorly visualised. The LV was compressed by the RV (Figure 2A). RV enlargement and slight impairment of contractility were observed. Pulmonary regurgitation was mild. A 24-h Holter ECG showed no serious arrhythmia. Contrast-enhanced CT showed a narrowing in the RVOT near the patch and calcification of the nearby endocardium on the epicardial side (Figure 1B,C). No significant narrowing was detected in the RV other than at the site of the MVOP. There were no atherosclerotic changes and no aortic enlargement. Cardiac MRI showed that the RV end-systolic volume index was 75.9 ml/m2 and the RV ejection fraction was 30.9%. The regurgitant fraction at the pulmonary valve was 15.7%.
Although we considered that the patient’s symptoms may have been caused by RVOTO, it was difficult to obtain clear echocardiographic images of the RVOT and to calculate the pressure gradient at the RVOT in this patient. RHC was planned to evaluate the pressure gradient between the RV and pulmonary artery (PA) to determine the indication for surgical treatment of the RVOTO.
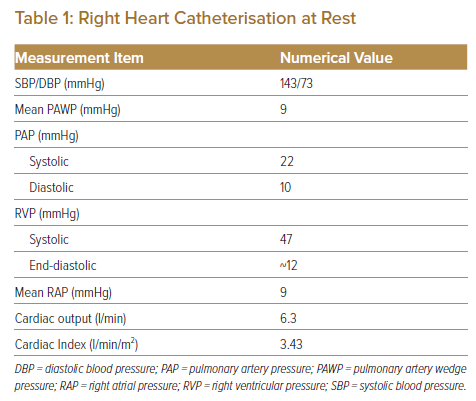
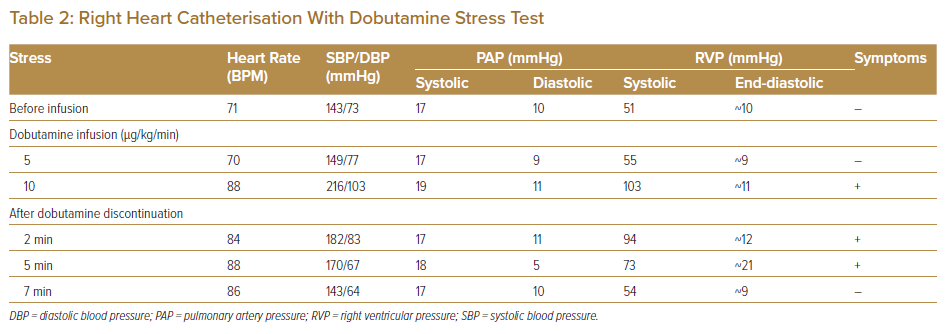
The RV–PA systolic pressure gradient was recorded as a peak-to-peak pressure gradient of 25 mmHg. The RV/LV systolic pressure ratio was 0.32 (Table 1). Because these data at rest did not meet the criteria for reoperation,2 we added a dobutamine stress test during RHC to evaluate the severity of RVOTO, following a protocol for the stress test established by the Japanese Society of Echocardiography.3 Dobutamine infusion was initiated at a rate of 5 μg/kg/min and increased at 5-min intervals to 10, 20, 30 and 40 μg/kg/min until one the following termination criteria is met: a target heart rate of (220 − age) × 0.85 (BPM); a significant decrease or increase in systolic blood pressure (≤80 or ≥220 mmHg); manifestation of significant tachyarrhythmia; or manifestation of intolerable symptoms. The dobutamine stress test was performed in the cath lab to facilitate an emergency response because the patient’s symptoms, including syncope, placed him at high risk.
Infusion of dobutamine at 10 μg/kg/min increased systolic RV pressure without changing PA pressure, and the RV–PA pressure gradient increased to 84 mmHg. In association with these haemodynamic changes, the patient felt the same symptoms as those on exertion, and the dobutamine stress test was terminated. Following termination of the dobutamine infusion, the patient’s symptoms improved and his systolic RV pressure decreased (Table 2). The stress test was not associated with serious arrhythmia.
Based on these findings, we considered that the indication for reoperation of RVOTO after TOF repair was met. The patient underwent pulmonary valve replacement and RVOT patch reconstruction. He was discharged 11 days postoperatively with no complications. His subjective symptoms during exertion improved significantly, and syncope did not recur. An exercise stress test was performed before discharge, and no symptoms were observed, even when the systolic blood pressure was around 200 mmHg. Echocardiography 3 months postoperatively showed that the RV overload was improved (Figure 2B) and that the tricuspid regurgitation pressure gradient had dropped to 22 mmHg. The RV diameter decreased from 43.7 to 31.9 cm.
Discussion
The most common cause of death in patients with repaired TOF is reportedly sudden cardiac death caused by ventricular tachycardia and fibrillation.4 Thus, the cause of syncope should be identified to avoid sudden cardiac death. In the present case, a 24-h Holter ECG revealed no serious arrhythmia, and resting RHC data did not meet the criteria for reoperation of RVOTO.
Because we suspected that the RV–PA pressure gradient may increase during exertion with reference to the patient’s medical history, we added a dobutamine stress test during RHC. This unmasked the changes in the severity of the RVOTO and reproduced the same symptoms as experienced by the patient during exertion without serious arrhythmia; therefore, it seemed reasonable to assume that the cause of the syncope and symptoms during exertion was RVOTO. Our strategy was supported by the relief of the patient’s symptoms after the reoperation. Medical treatment, such as a beta-blockers, may be suitable for mild symptoms due to dynamic obstruction. However, our patient’s symptoms were severe with syncope, and the effect of drug treatment was likely limited considering the mechanism of stenosis inferred by the CT imaging.
It was important to consider the mechanism underlying the changes in the severity of RVOTS to decide whether RVOT myectomy was required in addition to pulmonary valve replacement and RVOT patch reconstruction. In this case, CT showed calcification in the MVOP but no muscular obstruction in the RVOT. These findings were also confirmed intraoperatively.
LV outflow tract obstruction provoked by the dobutamine stress test has been reported as an independent predictor of future episodes of syncope.5 However, few reports have evaluated the usefulness of the stress test to assess RVOTO, and guidelines provide no recommendations for the stress test in adults with congenital heart diseases. Hasan et al. reported that exercise stress echocardiography was useful in evaluating the effects of labile RVOTO on RV function in patients with repaired congenital heart diseases, most of which were TOF.6 Although stress echocardiography is less invasive than catheter-based examinations, this method is only applicable to patients in whom echocardiographic assessment of RVOT is feasible. An exercise stress test may be more physiological than a dobutamine stress test; however, life-threatening arrhythmia is a contraindication to an exercise stress test.3 Thus, a dobutamine stress test was used in our patient with syncope suspected to be due to potentially fatal arrhythmia.
Although a consensus has not been achieved regarding the risk factors for sudden cardiac death in patients with repaired TOF, several studies have suggested that RV dysfunction, RV enlargement and elevated RV systolic pressure are risk factors.7 Labile RVOTO is likely to elevate RV systolic pressure on a daily basis, resulting in RV enlargement and dysfunction. Postoperative echocardiography in our case showed a decrease in RV volume and systolic pressure. Thus, in addition to the relief of dyspnoea and syncope on exertion, the reoperation for RVOTO may have helped prevent sudden death in our patient.
When considering the dobutamine stress test for adults with TOF, the risk of a sudden rise in blood pressure should be kept in mind, because such patients may have advanced aortic disease for their age.8 Even if there is no history of hypertension or obvious aortic enlargement, close attention should be paid to the dose of dobutamine, considering the potential aortopathy associated with TOF.
Recent studies have suggested the usefulness of novel methods to evaluate the severity of repaired TOF.9,10 Future studies are necessary to establish the indications for reoperation in patients with and without RVOTO.
Conclusion
In this study, RHC with a dobutamine stress test revealed the severity of labile RVOTO not found at rest in a patient with repaired TOF, and the stress test reproduced his symptoms on exertion. The results of the stress RHC were helpful in determining the need for reoperation, and the reoperation resulted in an improvement in the patient’s symptoms, with a decrease in RV systolic pressure and volume. When RVOTO is suspected to cause symptoms and/or progression of RV dysfunction but the indications for reoperation are not met, a stress test may be useful in evaluating the effects of labile RVOTO.
Clinical Perspective
- RVOTO is a residual complication in patients with repaired TOF, with the number of reoperations in adulthood increasing.
- Although current guidelines provide indications for reoperation of RVOTO, they do not necessarily cover all patients who are eligible for reoperation in terms of prevention of sudden death and preservation of RV function.
- Dobutamine stress RHC may be useful when RVOTO is suspected to be the cause of serious symptoms but the indications for reoperation are not met during the examination at rest.